Sarcoma is one of the rarest kinds of cancer but also one of the most severe ones. Sarcomas are different from other various types of cancer as it develops in the most different type of tissue. it occurs in the connective tissue of the body. Connective tissue is a type of group of cells that contributes towards connecting and supporting different kinds of tissues in your body. Common connective tissues in our body include blood vessels, fat, muscles, deep skin tissue, nerves, bones, fat and cartilage.
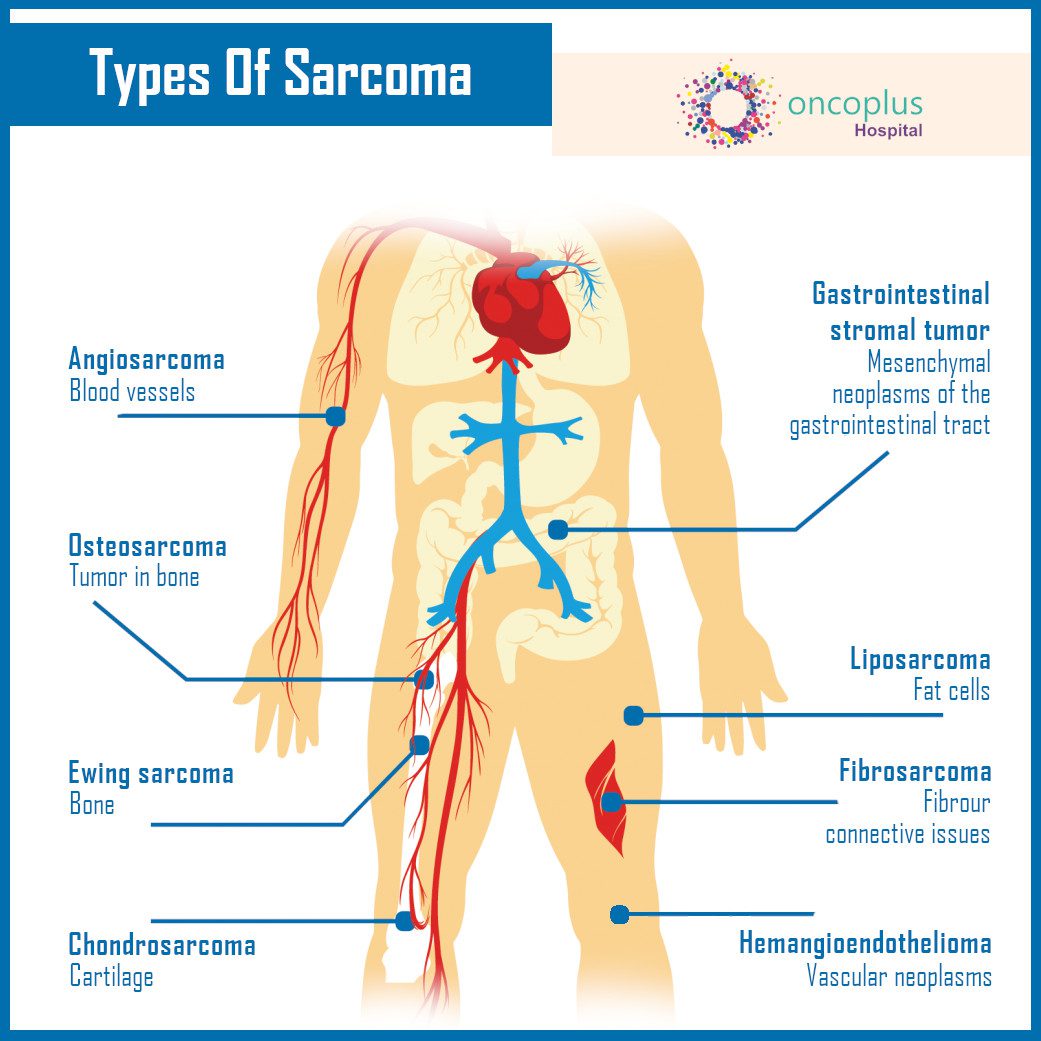
Sarcomas are not only present in the bones, muscles, tendons and other connective tissue, they can develop in other parts of the body as well. it is just a general term used for connective tissue and bone tumour. There are more than 50 different types of sarcoma but they are mainly divided into two common groups based on the location of their occurrence.
There are several treatment options available to cure bone cancer at Oncoplus Hospital, Delhi.
Types
it is differentiated into two main kinds: Soft tissue (Connective tissue) Sarcoma and Osteosarcoma (Bone Sarcoma). Sarcoma is very rare in adults but it does develop in both adults and children. Here is one of the most common types of sarcoma of soft tissue and Osteosarcoma:
- Leiomyosarcoma: Affects smooth muscle in organ walls, often in the abdomen.
- Gastrointestinal stromal tumour: Affects specialized gut neuromuscular cells
- Synovial sarcoma: Stem cells tumour where cancerous tissue develops around the joints
- Liposarcoma: Affects the fat cells in soft tissue. It occurs inside the thigh or in the retroperitoneum.
- Neurofibrosarcoma: Affects the protective lining of the nerves.
- Angiosarcoma: Affects the blood or lymph vessels.
- Rhabdomyosarcoma: Occur in skeletal muscle.
- Vascular sarcoma: Affects blood vessels.
- Fibrosarcomas: Affect fibroblast which is the most common cells of connective tissue
- Myxofibrosarcoma: Affects the connective tissue. Develops around the arms and legs of older adults.
- Mesenchymal: Extremely rare. Affects any part of the body.
- Schwannoma: Affects the tissues that cover the nerves.
- Kaposi’s sarcoma: Affects the skin mostly but can develop elsewhere.
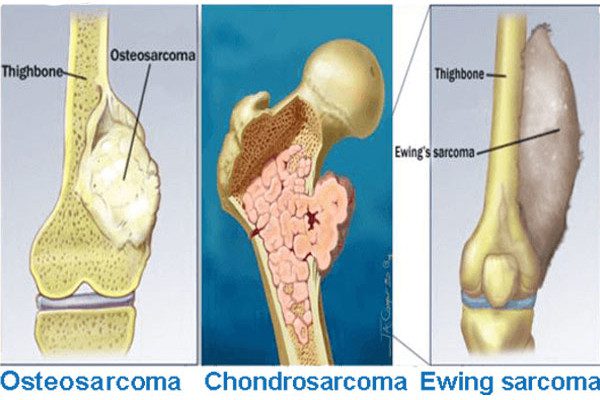
- Osteosarcoma (Sarcoma of the bone)
- Chondrosarcoma: Affects the cartilage.
- Fibrosarcoma: Affects fibrogenic tissue.
- Ewing sarcoma: Affects the bone or soft tissue.
Symptoms
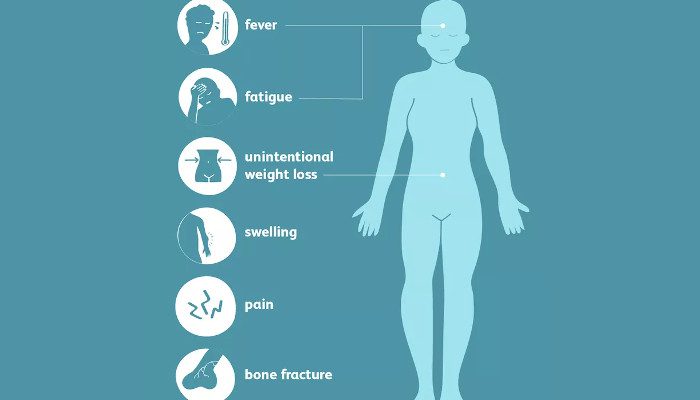
Sarcoma is differentiated into two groups and each shows different symptoms of their development. However, the soft tissue sarcomas are hard to identify as they can develop in any region of the body. However, some helpful signs are still there in its development. Here are some of the most common ones:
- Uncomfortable while breathing
- Presence of noticeable lump which is usually not painful in the beginning.
- Increase in the size of swelling or lump that affects the nerves or muscle
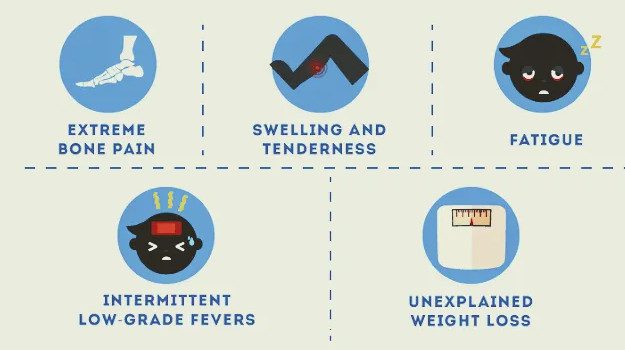
- Symptoms of Bone Sarcoma
Compared to tissue sarcoma, osteosarcoma is pretty visible and it develops quite early. Here are some of the most common symptoms of bone sarcoma:
- Pain in the body around the affected bone
- Excessive soreness and aching in bones especially at night
- Noticeable and painful swelling
- Develop a limit if it occurs in your leg
Osteosarcoma is quite prevalent in youngsters and children than adults. Hence if you experience such symptoms, don’t always mistake them for casual pain or swelling from sports or games. It’s usually bigger than that and if you experience the pain majorly at night then ask for immediate help and support from your doctors.
Book an appointment with the best oncologists for cancer treatment as well as diagnosis at best cancer Hospital in Delhi.
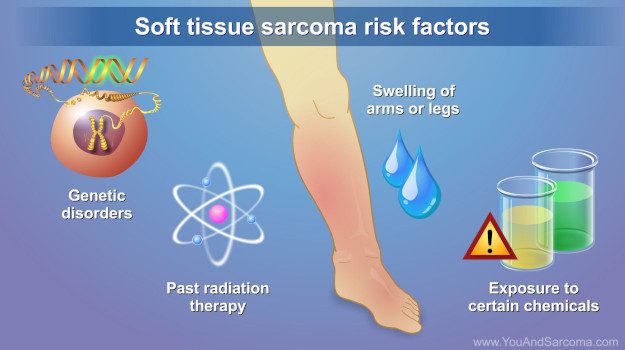
Risk Factor of Sarcoma
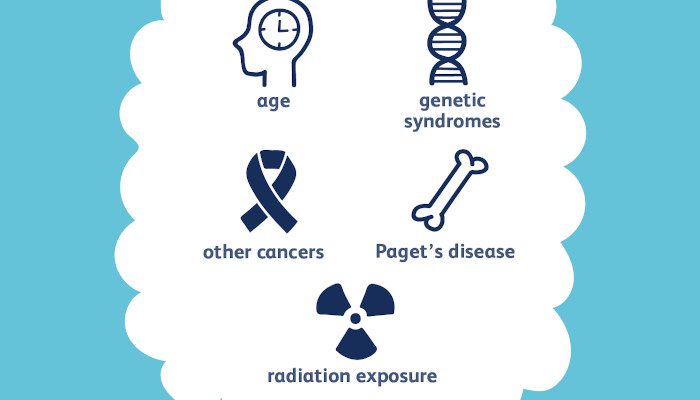
The cause of the Sarcoma is still unclear to researchers and scientists working on its development. However, some suggestive risk factors can contribute towards its leading cause.
Here are some noteworthy risk factors that increase the rate of sarcoma occurrence in the human body:
- Inherited Syndromes: Inheritance of any cancerous disease plays a consequential part on the progeny or the next generation. If there are syndromes like familial retinoblastoma and neurofibromatosis type 1 in your family then, unfortunately, you have a higher chance of developing sarcoma.
- Chemical Inhalation or Use: Harmful chemicals also contribute to sarcoma growth. Hence if you live under the exposure of Industrial chemicals then there's a higher risk of developing sarcoma that mainly affects the liver.
- Radiation therapy for cancer: If you’ve undergone radiation treatment for cancer then there’s a risk of developing sarcoma later in life.
- Exposure to Virus: The virus called herpesvirus 8 is also one of the biggest reasons behind the contribution of sarcoma. It causes Kaposi’s sarcoma which is a type that weakens the immune symptoms and makes you more prone to deadly diseases.
- Lymphedema: Lymphedema is a condition where swelling occurs due to the backup of lymph fluid when there's a blockage in the lymphatic system which leads to the risk of developing angiosarcoma (as discussed above).
Diagnosis
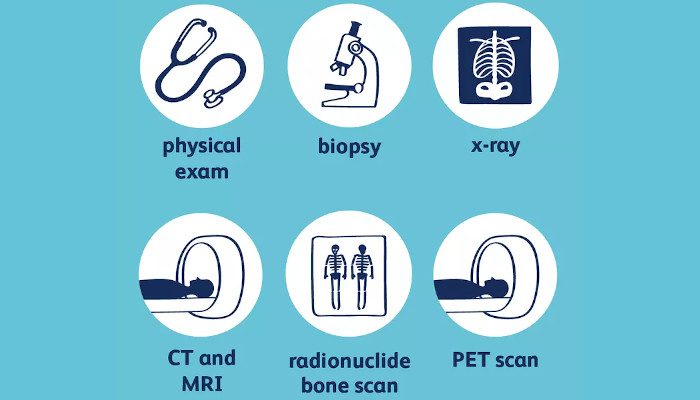
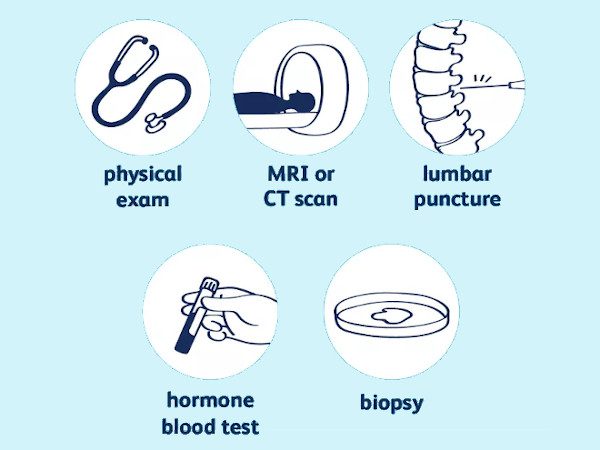
The diagnosis of sarcoma is done by various tests and procedures to comprehend the various stages of tumour development. Here are some of the common diagnostic steps for sarcoma identification:
- Physical Exam: Physical exams consist of checking the changes in the body such as the development of the lumps and other noticeable symptoms of sarcoma.
- Biopsy: Biopsy is a procedure that involves inspection of the suspicious tissue for lab testing to determine any growth signs and symptoms.
- Scans and other Imaging Tests: Imaging tests help to recognize the change in the body through X-rays and other tests depending on your situation. Imaging tests like MRI are helpful in identification of connective tissue problems. While other tests like ultrasound, scans and positron emission tomography scan also help to identify sarcoma better.
Biopsy is done by either piercing a needle through the skin or cutting away the tissue during operation depending on its location.
Treatment options of Sarcoma avialable at Oncoplus Hospital,Delhi.
Sarcoma is majorly treated by surgery through removing cancer. However, other treatments are used after or before the surgery. Not all surgery types work on all sarcoma as each one is different based on their situation. Here are some of the most common treatment for sarcoma:
Surgical Operation
Surgery helps to remove the cancerous cells of the sarcoma hence stopping it from spreading to the rest of the body. Sometimes when the condition is severe then there’s a need to amputate the arm or the leg of the body to stop cancer from growing to the other parts of the body. However recently the surgeons are trying to preserve the limp function to the extent that is possible. Surgical operation for sarcoma also results in hurting significant structures in the body such as nerves and organs to remove the sarcoma to the best way possible.
Chemotherapy
It’s one of the most common ways to treat cancerous cells through drug treatment with the help of chemicals to kill the growing cells. Chemotherapy can help with treatment for some types of sarcoma to stop its growth.
Radiation Therapy
Its a type of cancer treatment that involves the use of beams of intense energy to kill the growing cancerous cells in the body. Radiation therapy uses X-rays and also protons and other types of energy to neutralise the growing disease. It’s an external therapy where the radiation comes from the machine and moves around your body.
Immunotherapy
It’s a drug treatment that works by strengthening the immune system enough to fight out the cancerous cells.
Ablation Therapy
Ablation therapy involves destroying cancerous cells by the use of electricity to heat the cells, or use extreme cold liquid to freeze the cells. Even high-frequency ultrasound waves are also used to destroy the damaging cells to remove the growing tumour.
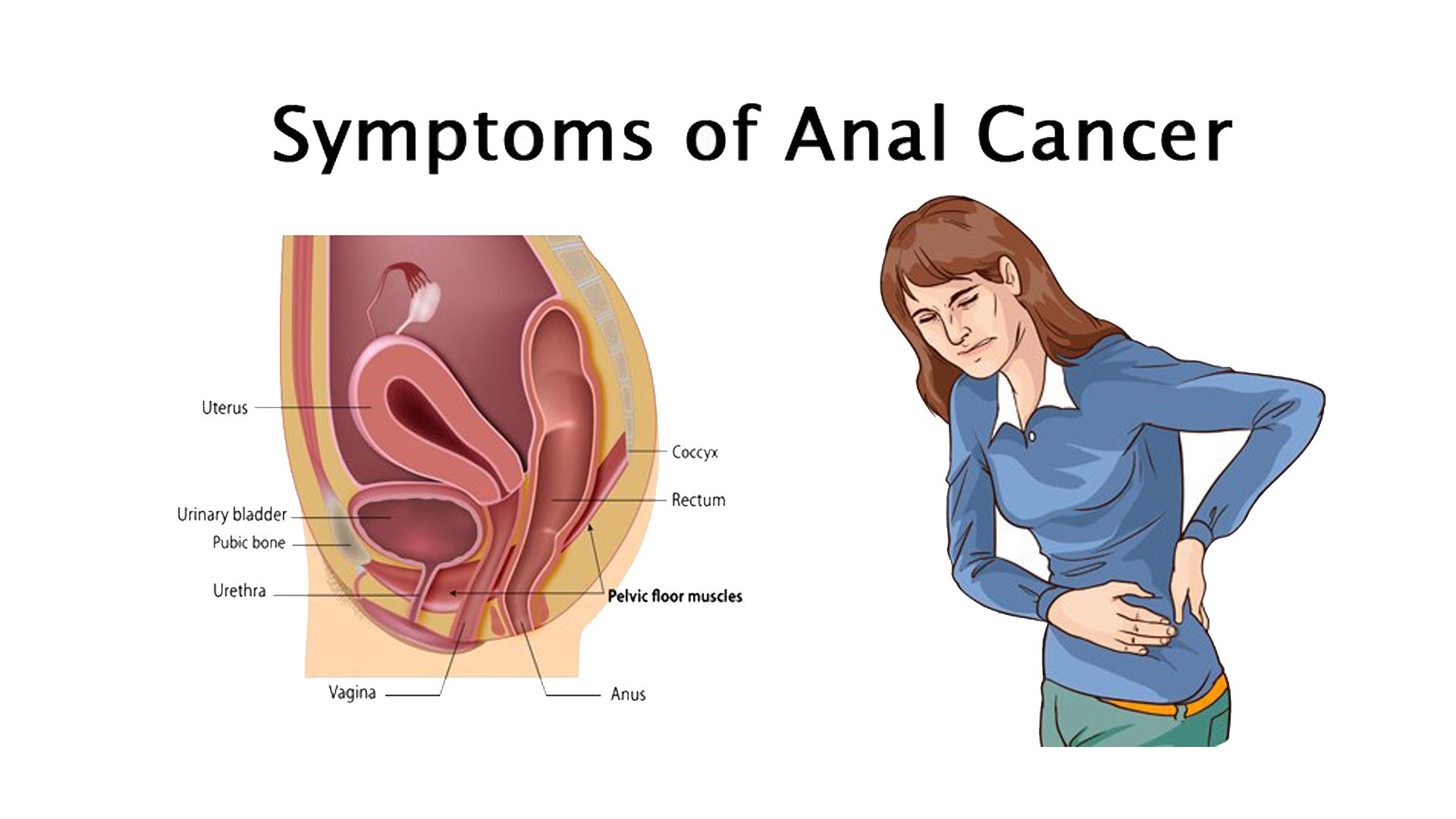
ANAL CANCER
Anal cancer is an uncommon type of cancer that occurs in the anal canal. The anal canal is a short tube at the end of rectum through which stool leaves the body.
In anal cancer, cancer (malignant) cells form in the tissues of the anus.
It is estimated that, around 50% of all the anal cancers are diagnosed before the cancer has spread beyond the primary site, and approximately 80% of all anal cancers are diagnosed in persons above 60 years old.
Cancer begins when some cells divide abnormally without stopping. As the cancer grows, it can be limited upto nearby tissues while in some cases, can spread to other parts of the body.
There are several treatment options available to cure bone cancer at Oncoplus Hospital, Delhi.
Symptoms
Signs and symptoms of anal cancer include:
- A feeling of fullness around the anus
- Pain in anal region
- Long lasting anal itching
- Bleeding from the anus or rectum
- A mass or growth in the anal opening
- Unusual discharges from the anus
- Change in bowel habits
- lumps that look like as haemorrhoids or piles
- narrow stools
- swollen lymph nodes in the groin or anal area
- Feeling like you constantly need to have a bowel movement.
If you experience any of the above symptoms, you should consult our oncology experts at Oncoplus Hospital, Delhi.
Preventive measures for anal cancer
There are no certain ways by which anal cancer can be prevented but there are certain measures, that can definitely help reducing the risk of anal cancer. Most common preventive ways are listed below:
- Stop smoking: Smoking increases the risk of anal cancer like any other cancer.
- HPV vaccines: Certain HPV infections can be protected with the help of vaccine. Some vaccines protect against certain type of HPV infection, while some vaccines protect against HPV infections including some types that cause anal and genital warts.
These vaccines if given before a person becomes sexually active, can help prevent HPV infection. - Condom use: Condoms may provide some protection against HPV (and HIV), but they don’t prevent infection completely.
Condoms if used correctly these can lower the genital HPV infection rate in women, hence should be used while every sexual activity. However, condoms cannot protect completely because they do not cover every possible HPV-infected area of the body, like the genital or anal area. - Limit sexual partners: It is advised to practice safe sexual activity, it can be practiced by limiting the number of sexual partners, using condoms during sex and getting tested regularly for sexually transmitted infections.
Book an appointment with the best oncologists for cancer treatment as well as diagnosis at best cancer Hospital in Delhi.
Treatment
There are certain treatment options available for anal cancer, these options depend on certain factors such as, stage of the cancer and overall health of the patient.
Surgery
Oncology experts at Oncoplus Hospital, Delhi typically use different procedures to remove anal cancer based on the stage of the cancer:
- Resection: In this procedure, the surgeon removes a small tumour along with some surrounding tissue. This procedure is done in the cases where cancer has not affected the anal sphincter or muscle. This procedure helps the patient to have a normal bowel movement.
- Abdominoperineal resection: In this procedure, the surgeon removes the anus, rectum, and a section of the bowel. The patient would not be able to have a normal bowel movement, therefore, the surgeon constructs a colostomy. A patient with a new colostomy can lead a normal life, can play sports and can be sexually active.
Combined chemotherapy and radiation
Oncology experts at Oncoplus Hospital, Delhi usually treat anal cancer with a combination of chemotherapy and radiation. These two treatments together enhance each other and improve chances for a cure.
- Chemotherapy: Chemotherapy is given with the help of medicines in the form of pills also through veins termed as intravenous. These drugs destroy rapidly growing cancerous cells. However, chemotherapy has its own side effects as these drugs also damage healthy cells that grow rapidly, including those in the receiver’s gastrointestinal tract and hair follicles. Side effects as a result of chemotherapy include nausea, vomiting and hair loss.
- Radiation therapy Radiation therapy kill cancer cells using high-powered radiations, such as X-rays and protons. In the process of radiation therapy, the patient is made to lie on a table and radiations are directed to specific areas of patient’s body to target the cancer cells.
Radiation therapy for anal cancer is usually given for five to six weeks. Oncologist defines the treatment schedule based on the type and stage of the cancer and patient’s general health.
A combination of both treatments procedures chemotherapy and radiation increases the effectiveness of the treatment.
Immunotherapy
Immunotherapy is a mode of treatment for any cancer that uses the patient’s immune system to conquer cancer. Immunotherapy works by interfering with that process of patient’s body that makes patient unable to attack the cancer cells by blinding his/her immune system.
Palliative / Supportive care
Palliative care is specialized medical care that focuses on providing relief from pain and other symptoms of a serious illness such as cancer. Palliative care team include doctors, nurses and other specially trained professionals, these specialists work with patient, his/her family and other doctors of patient to provide an extra layer of support that complements the patient’s ongoing care. Palliative care teams aim to improve the quality of life for people with cancer and their families. This form of care is offered alongside curative or other treatments patient may be receiving.
Palliative care can be used parallelly with other undergoing aggressive treatments, such as surgery, chemotherapy or radiation therapy. When palliative care is used along with all of the other appropriate treatments, patients with cancer may feel better and live longer.
Brain cancer is a cancerous growth of abnormal brain cells in the brain. Some brain tumours are benign/non-cancerous while some are malignant/cancerous. There are several different types of tumours that occur in the brain and the spinal cord. The brain is the central organ governing other organs and systems in the body, so all brain tumours need not to be ignored.
Benign tumours are those, that do not invade nearby tissue or spread to distant areas. While, malignant tumours grow and spread aggressively, overpowering healthy cells by taking their space, blood, and nutrients. Malignant tumours can also spread to distant parts of the body.
There are several treatment options available to cure bone cancer at Oncoplus Hospital, Delhi.
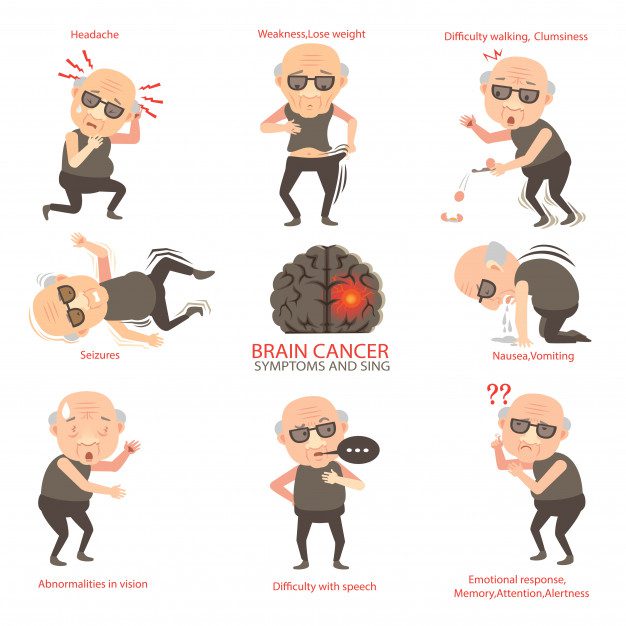
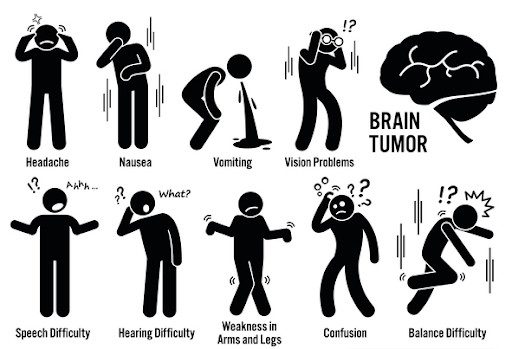
Signs and Symptoms of Brain cancer
The signs of a brain tumour depend on the size of brain tumour, location and rate of tumour’s growth. Typical signs and symptoms any patient of brain tumours may experience, include:
- Change in pattern of headaches
- Frequent and severe headaches
- Nausea or vomiting
- Problems related to vision problems including blurred vision or double vision
- Loss of sensation or movement in an arm or a leg gradually
- Physical weakness
- Difficulty in speaking
- Getting confused in routine simple matters
- Changes in behaviour
- Seizures
- Difficulty in hearing
- Difficulty in normal walking or vertigo
- Problems with concentration, memory, attention, or alertness
- Changes in emotional response
Causing factors of Brain cancer
Many different types of primary brain tumours exist. Each gets its name from the type of cells involved. Examples include:
- Gliomas: These tumours begin in the brain or spinal cord and include astrocytomas, ependymomas, glioblastomas, oligoastrocytomas and oligodendrogliomas.
- Meningiomas: A meningioma is a tumour that arises from the membranes that surround patient’s brain and spinal cord (meninges). Most meningiomas are noncancerous.
- Acoustic neuromas (schwannomas): These are benign tumours that develop on the nerves that control balance and hearing leading from patient’s inner ear to patient’s brain.
- Pituitary adenomas: These are mostly benign tumours that develop in the pituitary gland at the base of the brain. These tumours can affect the pituitary hormones with effects throughout the body.
- Medulloblastomas: These are the most common cancerous brain tumours in children. A medulloblastoma starts in the lower back part of the brain and tends to spread through the spinal fluid. These tumours are less common in adults, but they do occur.
- Germ cell tumours: Germ cell tumours may develop during childhood where the testicles or ovaries will form. But sometimes germ cell tumours affect other parts of the body, such as the brain.
- Craniopharyngiomas: These rare, noncancerous tumours start near the brain's pituitary gland, which secretes hormones that control many body functions. As the craniopharyngioma slowly grows, it can affect the pituitary gland and other structures near the brain.
Book an appointment with the best oncologists for cancer treatment as well as diagnosis at best cancer Hospital in Delhi.
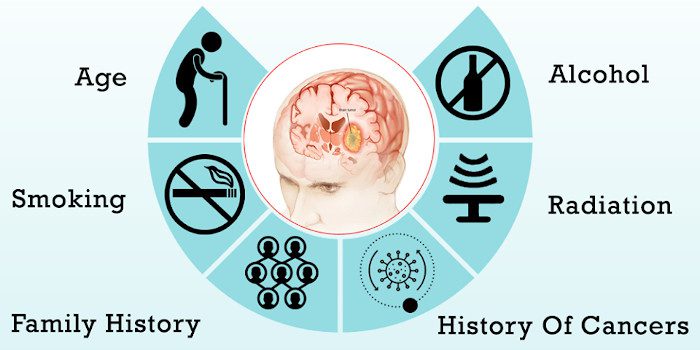
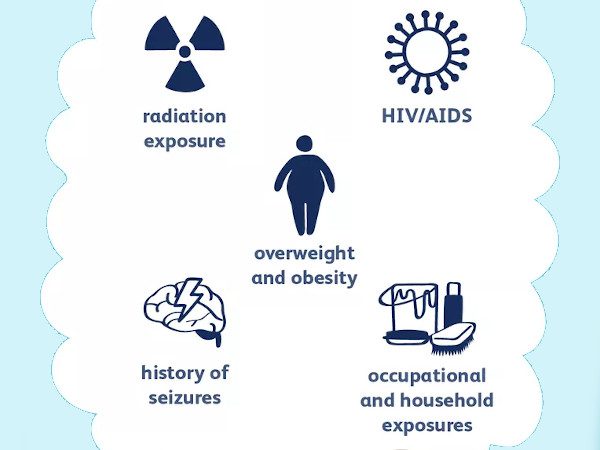
Risk factors
In most patients with primary brain tumours, the cause of the tumour is not clear. But doctors have identified some factors that may increase patient’s risk of a brain tumour.
- Exposure to radiation: Patients who have been exposed to a type of radiation called ionizing radiation have an increased risk of brain tumour. Examples of ionizing radiation include radiation therapy used to treat cancer and radiation exposure caused by atomic bombs.
- Family history of brain tumours: A small portion of brain tumours occurs in patients with a family history of brain tumours.
- Age: Brain tumours are more common in children and older adults, although patients of any age can develop a brain tumour.
- Gender: In general, men are more likely than women to develop a brain tumour. However, some specific types of brain tumours, such as meningioma, are more common in women.
- Home and work exposures: Exposure to solvents, pesticides, oil products, rubber, or vinyl chloride may increase the risk of developing a brain tumour.
- Exposure to infections, viruses, and allergens
- Ionizing radiation: Previous treatment to the brain or head with ionizing radiation, including x-rays, has been shown to be a risk factor for a brain tumour.
- Head injury and seizures: Serious head trauma has long been studied for its relationship to brain tumours. A history of seizures has also been linked with brain tumours, but because a brain tumour can cause seizures, it is not known if seizures increase the risk of brain tumours, if seizures occur because of the tumour, or if anti-seizure medication increases the risk.
Diagnosis
A number of tests and procedures are recommended to rule out the diagnosis.
- A neurological exam: A neurological exam may include checking:
- patient’s vision,
- hearing,
- body balance,
- coordination,
- strength and reflexes.
- Magnetic resonance imaging: MRI is commonly used to help diagnose brain tumours.
- Biopsy: A biopsy can be performed as part of an operation to remove the brain tumour, or a biopsy can be performed using a needle. The biopsy sample is then viewed in a laboratory under a microscope to determine if it is cancerous or benign.
- CT scan: A CT scan takes pictures of the inside of the body using x-rays taken from different angles that shows any abnormalities also size of tumour if present. A CT scan can help find bleeding and enlargement of the fluid-filled spaces in the brain, called ventricles.
- Positron emission tomography (PET) or PET-CT scan: A PET scan is used at first to find out more about a tumour while a patient is receiving treatment. It may also be used if the tumour comes back after treatment.
- Cerebral arteriogram is also called a cerebral angiogram: A cerebral arteriogram is an x-ray, or series of x-rays, of the head that shows the arteries in the brain. X-rays are taken after a special dye called a contrast medium is injected into the main arteries of the patient’s head.
- Lumbar puncture or spinal tap: A lumbar puncture is a procedure in which a needle is used to take a sample of cerebrospinal fluid to look for tumour cells, blood, or tumour markers. Tumour markers or biomarkers are substances found in higher than normal amounts in the blood, urine, spinal fluid, plasma or other bodily fluids of patients with certain types of tumours.
- Myelogram: The doctor may recommend a myelogram to find out if the tumour has spread to the spinal fluid, other parts of the brain, or the spinal cord. This is rarely done.
- Neurocognitive assessment: This consists of a detailed assessment of all major functions of the brain including storage and retrieval of memory, expressive and receptive language abilities, calculation, dexterity, and the overall well-being of the patient. These tests are done by a licensed clinical neuropsychologist.
- Electroencephalography (EEG): An EEG is a non-invasive test in which electrodes are attached to the outside of a patient's head to measure electrical activity of the brain. It is used to monitor for possible seizures.
Treatment Options for Brain cancer available at Oncoplus Hospital, Delhi
Treatment for a brain tumour depends on the type, size and location of the tumour, as well as patient’s overall health. Treatment methods commonly used are explained below:
Surgery
If the brain tumour is located in a place that makes it accessible for an operation, patient’s surgeon will work to remove as much of the brain tumour as possible.
In some cases, tumours are small and easy to separate from surrounding brain tissue, which makes complete surgical removal possible. Whereas, in other cases, tumours cannot be separated from surrounding tissue or they are located near sensitive areas in patient’s brain, making surgery risky. In these cases, the surgeon removes as much of the tumour as is safe.
Radiation therapy
Radiation therapy destroys cancer cells using high-energy beams, such as X-rays or protons.
External beam radiation can focus just on the area of patient’s brain where the tumour is located, or it can be applied to patient’s entire brain in case where cancer has spread to the brain from some other part of the body and forms multiple tumours in the brain.
Chemotherapy
Chemotherapy involves medicines to destroy cancer cells. Chemotherapy drugs can be consumed orally by the patient in pill form or can be injected into a vein. Many chemotherapy drugs are available and may be used depending on the type of cancer.
Chemotherapy side effects depend on the type and dose of drugs patients receive. Chemotherapy can cause nausea, vomiting and hair loss.
Tests of patient’s brain tumour cells can determine whether chemotherapy will be helpful for patients. The type of brain tumour patients have also is helpful in determining whether to recommend chemotherapy.
Targeted drug therapy
Targeted drug treatments aim at destroying cancer cells by identifying and blocking specific abnormalities present within cancer cells.
Targeted therapy drugs are available for certain types of brain tumours, and many more clinical trials are ongoing.
Life of Cancer Patient After Survival
A cancer survivor is that the patient who had cancer and has been cured in real time. Patients who have survived cancer may expect to travel back to their normal lives.
With advancement of diagnostic tools cancer survival rate has been improved in times as compared to what it's going to are 20 years ago. However, still some cancers are more survivable than other types.
Higher survival rates could also be thanks to the subsequent major improvements in cancer prevention and treatment:
Screening tests may find cancers earlier. These tests include:
- Mammography for carcinoma
- PSA for prostatic adenocarcinoma
- Colonoscopy for colorectal cancer
- pap smear for cervical cancer
- Existing treatments are getting used in better ways
- Less side effects, which keeps planned treatments on schedule
- Newer treatments like targeted therapy and immunotherapy
There are several treatment options available to cure bone cancer at Oncoplus Hospital, Delhi.
Understanding survivorship
Cancer survivorship has a minimum of 2 common meanings:
- Having no signs of cancer after completing treatment.
- Cancer survivorship typically starts at diagnosis. It includes patients who receive treatment over a extended time. Their treatment can lower the prospect of the cancer returning or help to contain the cancer from spreading to other organs in body.
Book an appointment with the best oncologists for cancer treatment as well as diagnosis at best cancer Hospital in Delhi.
There are 3 phases of survivorship:
- Acute survivorship: starts at diagnosis and aims at completing the initial cancer treatment.
- Extended survivorship: focuses on the consequences of cancer and treatment. It starts at the top of initial treatment and goes through an extended time- the months after.
- Permanent survivorship: focuses on Long-term effects of cancer and treatment is when years have passed since cancer treatment ended. there's less of an opportunity that the cancer may come.
Living with a history of cancer is different for every patient. But most patients have the common belief that life is different after cancer.
At the top of treatment, survivors may have the subsequent concerns:
- Appreciating life more.
- Being more accepting of themselves.
- Feeling more anxious about their health.
- Not knowing the way to cope after treatment ends.
- A sense of relief that their treatment is over
- Not sure about their disease in future
- Increased anxiety and stress
- A fear that the cancer would come
- Physical, psychological, sexual or fertility problems
- Struggles with Relationship
- Discrimination at some workplaces
Life of cancer patients After Survival
Patients should have information about the psychological also social issues that they're getting to face once they return to home after completing their treatment.
Cancer is usually described as a journey that starts at diagnosis. During treatment, some patients feel that their life is on hold. After treatment ends, it's going to be hard to understand the way to resume normal activities.
Survivors may expect life to return to what it had been like before the cancer diagnosis. for several patients, though, it's not that straightforward . the truth is usually more emotionally and physically complex. Some cancer survivors find they can’t or don’t want to travel back to how life was before their treatment.
Many survivors say that cancer changes them. After treatment, they'll feel different, albeit they appear an equivalent. With time, survivors often find a replacement way of living. Some feel they ought to be happy and filled with wisdom because they survived, but instead feel guilty that this isn’t the case.
Some patients feel as if they need fought a battle and wish time to rest. Others want to return immediately to their previous life.How does a patient feel and cope up with the disease depends on the sort of cancer and treatment.
Many cancer survivors have ongoing health concerns thanks to the cancer or due to treatment. These may include fatigue, difficulty sleeping, pain and depression. The after-effects of treatment can make lifestyle difficult.
Certain major changes in such patients’ life are explained below:
Changes in relationships
When active treatment is over, some survivors’ needs change and relationships may shift. For example:
- Some friends may become closer, while others keep themselves at a distance.
- Families can become overprotective.
- Relationship problems from before the cancer diagnosis can surface again.
What you'll do:
- Understand that the whole family changes from the cancer experience in ways they'll not remember of.
- Work through these changes to urge the support you would like.
- Maintain open and ongoing communication.
Getting back to work
Going back to a daily work schedule may be a thanks to revisit to a traditional routine and lifestyle. most of the people need their job and therefore the insurance it provides.
People with cancer may:
- Work during treatment
- Take day off for treatment and return to figure when treatment ends
- Unable to return to figure thanks to the consequences of the cancer or its treatment
At work, you'll find that, Co-workers might want to assist but parallelly some employers are reluctant to rent someone who has had cancer due to fears the person won't physically be ready to handle work.
The Fertility Issue
Of the issues faced by cancer survivors, damaged fertility is one among the smallest amount understood. The side effects of radiation, chemotherapy, or surgery can leave a patient infertile.
Cancer patients can take special fertility-saving measures before treatment. Adult and adolescent males can make deposits during a depository for future use.
For women the problems are more complex. A woman's fertility-saving measures depend entirely on her cancer treatment and her particular physiology. Eggs are often extracted and frozen, as can embryos. From there, the measures become increasingly tailored to a private woman's needs.
That's why all women cancer patients who have the potential in touch a toddler got to see a fertility specialist during the cancer treatment. Oncologists at Oncoplus Hospital, Delhi encourage our female patients also as male patients to undergo fertility evaluation periodically while their treatment.
Word of advice by Oncoplus Team of oncologists
- Focus on every day and expect both good and bad days.
- Do things at your own pace. Plan rest time between activities. Avoid pressure to form decisions or start new activities immediately.
- Be prepared for mixed reactions from family and friends. If people don’t skills to react, try to not get upset. Some people avoid contact because cancer brings up difficult emotions. they're handling it in their own way.
- Share your feelings and worries with family and friends. Allow yourself time to regulate to those changes, and to elucidate to your friends and family that you simply need their support.
- Talk to your doctor if you're concerned about sadness or low moods.
- Practise some sort of relaxation, like meditation, visualisation, yoga or deep breathing.
- Keep a journal. many of us find it helps to write down down how they’re feeling.
- Join a support group. Speaking with other cancer survivors may assist you cope and cause you to feel more optimistic about the longer term . Learn from their experiences and mistakes.
- Attend a survivorship program, if there's one in your area.
- Read other survivors’ stories. Learning how people have made meaning of a cancer diagnosis may help.
Thyroid Cancer
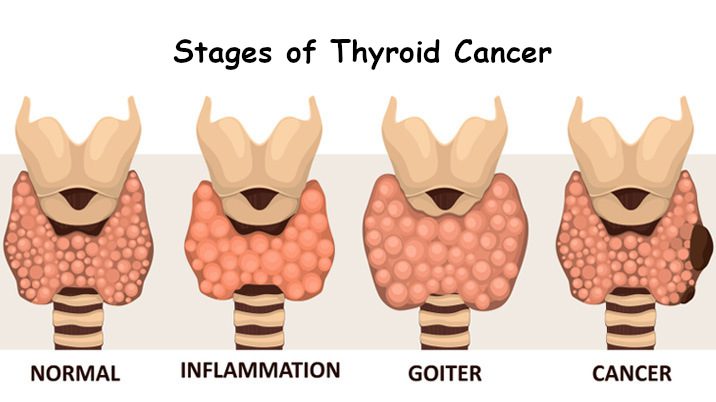
Thyroid is a small butterfly shaped gland situated at the base of neck. This gland controls our metabolism by producing those hormones that regulate heart rate, blood pressure, body temperature and body weight.
it develops in thyroid gland when cells change abnormally forming a tumour.
it might not show any signs at first but it can lead to severe pain associated with swelling in the neck.
Most cases can be managed with different treatment methods available.
There are several treatment options available to cure bone cancer at Oncoplus Hospital, Delhi.
TYPES
- Papillary thyroid cancer: This is the most common type of thyroid cancer. This type of cancer can occur at any age, but people between 30 to 50 years are affected most.
- Follicular thyroid cancer: Follicular thyroid cancer affects people older than age 50.
- Anaplastic thyroid cancer: Anaplastic is a rare type of thyroid cancer that occurs in adults age 60 and older. This can be the most severe type, because it spreads to other parts of body aggressively however this cancer is rare.
- Medullary thyroid cancer: begins in thyroid cells, which produce the hormone calcitonin and the elevated levels of calcitonin in the blood can indicate medullary thyroid cancer at an early stage.
Book an appointment with the best oncologists for cancer treatment as well as diagnosis at best cancer Hospital in Delhi.
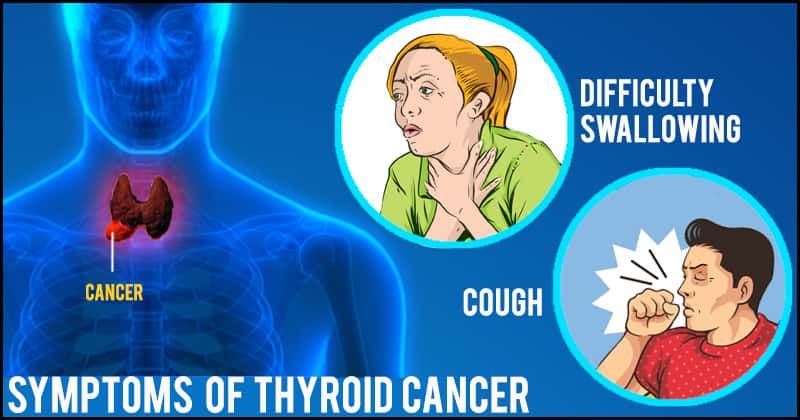
WHAT ARE THE SIGNS AND SYMPTOMS OF THYROID CANCER?
Initially, Thyroid cancer might not show any signs but it can lead to severe pain associated with swelling in the neck.
- Pain in neck and throat
- A lump in the neck
- Difficulty while swallowing
- Vocal changes causing hoarseness in voice
- Cough
CAUSES AND RISK FACTORS
Thyroid cancer develops when cells in the thyroid gland undergo certain genetic changes causing the cells to grow and multiply at fast rate. These cells accumulate abnormally forming a tumour.
However, there are several risk factors that contribute in the development of Thyroid cancer. These are:
- Gender: Women are three times more likely to get thyroid cancer than men
- Age: one can get thyroid cancer at any age. But women are often diagnosed in their 40s and 50s. Men tend to be older -- in their 60s and 70s -- when they find out they have it.
- Radiation Exposure: Children who get radiation therapy for some cancers, such as lymphoma, are at more risk of developing thyroid cancer. Adults exposed to radiation have lower chances of getting it when compared with children.
- Heredity and Genetics: The chances of getting thyroid cancer are higher if anyone in family had this disease.
- Not Enough Iodine in the Diet: Our body needs Iodine to make thyroid hormones. Certain thyroid cancers are more common in parts of the world where people have low levels of iodine.
HOW TO DIAGNOSE THYROID CANCER
Tests used to diagnose thyroid cancer are :
- Physical examination. The doctor examines neck to feel for physical changes in patient’s thyroid, such as thyroid nodules. He or she may also ask about the family history of thyroid tumors.
- Blood Tests. Blood tests help determine the functionality of the thyroid gland.
- Ultrasound. Ultrasound help the doctor to see if a lump is filled with fluid or it is solid. A solid lump is likely to contain cancerous cells. Further tests are required to confirm the diagnosis. The ultrasound also show the size and number of nodules on the thyroid.
- CT scan. CT Scan uses special X-rays to help the doctor a look inside the thyroid gland. body. It can show the size and location of thyroid cancer and whether it has spread to other parts of the body.
- Biopsy: Removing a sample of thyroid tissue. samples of suspicious thyroid tissue are removed using needles by the doctor and these samples are sent to the laboratory to look for cancer cells.
- Radioiodine scan. This scan measures the radiation in thyroid gland or other parts of patient’s body.
- PET Scan. This scan looks at the changes precisely using small amounts of radioactive material, called radiotracers, a special camera, and a computer to look closely at organs and tissue.
WHAT ARE THE STAGES OF it?
Papillary or Follicular Thyroid Cancer -- Patients below 45 years
- Stage I - Tumour may be of any size also it may have spread to nearby tissues but not to other parts of the body.
- Stage II - At this stage, cancer has spread to other parts of the body such as lungs or bones.
Papillary or Follicular Thyroid Cancer -- Patients above 45 years
- Stage I - The tumour is 2cm in size and limited to thyroid gland only.
- Stage II - Tumour is limited to the thyroid gland but size can be more than 2 cm upto 4 cm.
- Stage III - The size of tumour at this stage is larger than 4 cm and has spread to nearby tissues or nearby lymph nodes.
Stage IV is further divided into three categories:
- Stage IVA - The cancer has spread to skin, larynx, esophagus or trachea.
- Stage IVB - The tumor has grown upto spine or into nearby large blood vessels including carotid arteries. These arteries carry blood to face,brain and neck.
- Stage IVC - The cancer has spread beyond the thyroid upto lungs, bones, and distant lymph nodes.
TREATMENT OPTIONS
Treatment options for Thyroid cancer available at Oncoplus Hospital, Delhi are:
Surgery
Most people with thyroid cancer undergo surgery to remove the thyroid.
- Thyroidectomy: Removing all or most of the thyroid. A surgical intervention to remove the thyroid gland might involve removing all of the thyroid tissue or most of the thyroid tissue.
- Thyroid lobectomy: Removing a portion of the thyroid. During a thyroid lobectomy, the surgeon removes half of the thyroid. It might be recommended in case if patient has a slow-growing thyroid cancer in one part of the thyroid and no suspicious nodules exist in other areas of the thyroid.
- Lymph node dissection: Removing lymph nodes in the neck. The surgeon may also remove nearby lymph nodes in the neck while removing the thyroid.
Thyroid hormone therapy
After thyroidectomy, thyroid hormone medication may be recommended for some patients for life. This therapy is beneficial for patients as these medicines supply the missing hormone patient’s thyroid would normally produce, and suppress the production of thyroid-stimulating hormone (TSH) from the pituitary gland. Because a high TSH levels could stimulate any remaining cancer cells to grow.
Radioactive iodine
Radioactive iodine treatment uses large doses of a form of iodine that is radioactive, which is often used after thyroidectomy to destroy any remaining healthy thyroid tissue. Radioactive iodine treatment may also be used in case thyroid cancer recur.
Radiation therapy
Radiation therapy is given externally using a machine that aims high-energy beams, such as X-rays and protons, at precise points on the patient’s body.
Chemotherapy
Chemotherapy is a drug treatment that uses chemicals to kill cancer cells. Chemotherapy is typically given as an infusion through a vein. The chemicals travel throughout the patient’s body, killing quickly growing cells, including cancer cells.
Targeted drug therapy
Targeted drug treatments is a newer treatment that targets only certain parts of cancer cells, to slow or stop growth. This therapy focus on specific abnormalities present within cancer cells. By blocking these abnormalities, targeted drug treatments can cause cancer cells to die.
Injecting alcohol into cancers
Alcohol ablation is used in case of very small tumours, it involves injecting small thyroid cancers with alcohol using imaging such as ultrasound to ensure precise placement of the injection. This causes thyroid cancers to shrink.
Palliative or Supportive care
Palliative care is specialized medical care that focuses on providing relief from pain and other symptoms of a serious illness. Palliative care specialists work with patient and his/her family to provide an extra layer of support that complements his/her ongoing care.
skin is the outer covering of our body, and is the largest organ of the body with a surface area around 20 square feet.
The skin is composed of three main layers:
- The epidermis is the outermost layer of the skin. This layer serves as a barrier for infections forming a waterproof protective wrapping around the body surface.
- Underneath the epidermis another layer is “Dermis” that contains connective tissue providing cushions to the body, nerve endings that provide the sense of touch and heat, blood vessels, hair follicles and sweat glands.
- The hypodermis is the innermost layer which is also known as subcutaneous tissue. It is made of fat serving as padding and insulation for the body and connective tissue to attach the skin to bones and muscles.
There are several treatment options available to cure bone cancer at Oncoplus Hospital, Delhi.
WHAT IS SKIN CANCER?
Skin cancers are cancers that start in the skin cells.
it is developed when the abnormal growth of skin cells develops on skin which is exposed to the sun. However, it can also occur on those areas of skin which are not exposed to sunlight.
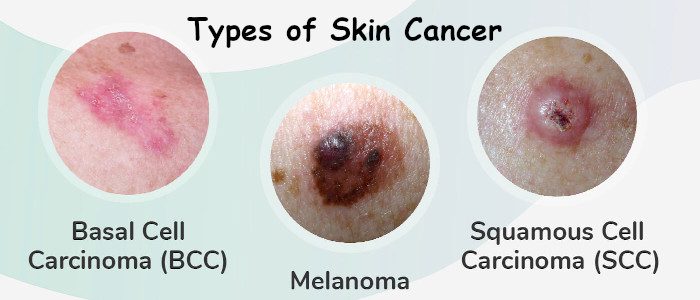
TYPES :
The outermost layer i.e, epidermis is made up of three types of cells- basal cells, squamous cells and melanocytes. Most common type of skin cancer develops in these tissues. These are as follows:
- Basal cell carcinoma: Basal cell carcinoma is rarely staged as these are almost always cured before they spread to other parts of the body.
- Squamous cell carcinoma: Squamous cell carcinoma usually occurs in the head and the neck regions and is more likely to recur and also spread to other parts of the body.
- Melanoma Skin Cancer: Melanoma is the cancer that starts in the melanocytes. These are skin cells that make a deep brown pigment called melanin which is responsible to give the skin its colour. It protects the deep layers of the skin from the effects of the sun and exposure to sun increases the production of melanin making people get tan or get darker.
Book an appointment with the best oncologists for cancer treatment as well as diagnosis at best cancer Hospital in Delhi.
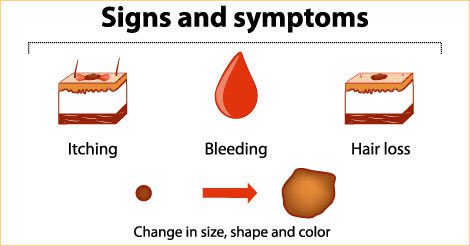
SYMPTOMS :
Skin cancer develops primarily on areas of sun-exposed skin, including the scalp, face, lips, ears, neck, chest, arms and hands, and on the legs in women. But it can also develop on palms, beneath fingernails or toenails, and genital area, that hardly see the sunlight.
The symptoms of the skin cancer can depend on the type of skin cancer too. The following are the symptoms of the common types of skin cancer:
- Sores or moles that appear smooth and pearly, look waxy or appear as a firm, red lump
- These may bleed sometimes
- They begin to heal but recurs
- These can be itchy too
- It may develop into a painless ulcer.
- A flat, flesh-coloured or brown scar-like lesion
- Red and scaly patches of the skin that bleed
- Bleeding sores
- A wart-like growth that bleed
- Itching, burning sensation and tenderness in the affected areas
- Changes in size, colour or feel of common (normal) moles
- Bleeding moles
- Brownish spot with dark speckles.
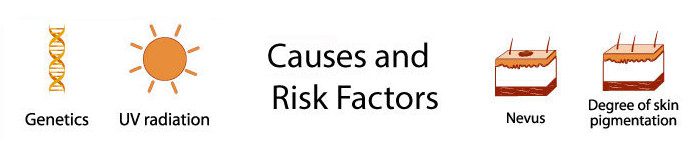
CAUSES
Skin cancer occurs when DNA of skin cells change, termed as mutation. This process cause the cells to grow abnormally forming a mass of cancer cells.
ULTRAVIOLET RAYS
Much of the damage to DNA in skin cells results from ultraviolet (UV) radiation found in sunlight and in the lights used in tanning beds. Ultraviolet (UV) radiation emitted by the sun can damage skin cells and genes, which makes it a major risk factor for skin cancer.
But sun exposure doesn't explain skin cancers that develop on skin not ordinarily exposed to sunlight. This indicates that other factors may contribute to the risk of skin cancer, such as being exposed to toxic substances or having a condition that weakens our immune system.
RISK FACTORS
Factors that may increase the risk of skin cancer include:
- Excessive sun exposure: People who spend more time in the sun might develop skin cancer. Excessive skin tanning is skin's injury response to excessive UV radiation.
- Sunny or high-altitude climates: People who live in sunny, warm climates are exposed to more sunlight are also at risk of developing skin cancer.
- Moles: People who have many moles or abnormal moles which look irregular and are generally larger than normal moles are at increased risk of skin cancer.
- Precancerous skin lesions: Having rough, scaly patches that range in colour from brown to dark pink skin lesions can increase the risk of developing skin cancer.
- A family history of skin cancer: If anyone in family once had skin cancer, one may be at increased risk of the skin cancer.
- A personal history of skin cancer: Patients with history of skin cancer can develop it again.
- A weak immune system: People with weakened immune systems tend to grow quickly and are more likely to cause death.
- Exposure to certain substances: Risk of skin cancer is more when exposed to certain substances, such as arsenic.
- HPV-Human papillomavirus can be related with a considerable amount of skin cancers.
Diagnosis:
- Physical examination: The Dermatologist examines the patient’s skin to determine whether the skin changes are likely to cause skin cancer. Further tests and investigations are required to confirm the diagnosis.
- Imaging Tests:
- Chest X ray
- CT scan
- PET scan
- MRI
- CT-PET scan
- Blood tests: Blood tests are done to check overall health of patient including marrow, liver, and kidney functions.
- Biopsy: “Dermatologist” removes the suspicious-looking skin for lab testing to determine whether you have skin cancer and, if so, what type of skin cancer it is.
STAGES :
Once it has been diagnosed, staging is done to determine the extent of the skin cancer in the body. Staging helps the “Oncologist or Cancer Specialist” to define the plan how to cure the cancer.
- Stage I: The cancer is around 2 cm or lesser in size and has no high-risk features.
- Stage II: The cancer is around 2 cm in size and has a few high-risk features.
- Stage III: The cancer spread into the bones of face like the jaw bone or the bone around the eye or it may grow to a nearby lymph node and size is less than 3 cm.
- Stage IV: The cancer has spread into the spine, lower part of the skull or the ribs or it has spread to a lymph node more than 3 cm in size or to an internal organ such as the lungs.
TREATMENT OPTIONS:
The following are the major treatment options available at Oncoplus Hospital, Delhi for treating skin cancers:
Skin Cancer Surgery
Surgery is the most common and preferred treatment method to cure skin cancer. There are different types of surgeries available to treat skin cancers, the exact type is chosen based on the severity of the condition and the location of the cancer.
- Mohs surgery: This procedure is for larger, recurring or difficult-to-treat skin cancers. This procedure allows cancerous cells to be removed without taking an excessive amount of surrounding healthy skin.
In this surgery, doctor removes the skin growth layer by layer, examining each layer under the microscope, until no abnormal cells remain. - Curettage and electrodessication: After removing most of a growth, the doctor scrapes away layers of cancer cells using a device with a circular blade (curet). An electric needle destroys any remaining cancer cells.
- Cryosurgery: Early it can be destroyed by freezing them with liquid nitrogen.
- Laser surgery:
- Excisional surgery: In this type of surgery doctor cuts out (excises) the cancerous tissue and a surrounding margin of healthy skin. A wide excision — removing extra normal skin around the tumor — may be recommended in some cases.
Targeted therapy
This treatment uses drugs that target the cancerous cells. They avoid causing extreme damage to the remaining healthy cells which can occur in chemotherapy. As a part of targeted therapy in treating recurrent basal cell carcinoma, a signal transduction inhibitor is used. These inhibitors block the signals that pass between molecules in the cells, which leads to death of those cells.
Immunotherapy
Immunotherapy aims in making the patient’s immune system stronger by using artificial substances to restore the body’s defence against cancer. This procedure is also known as biotherapy or biologic therapy.
Photodynamic therapy (PDT)
This treatment destroys skin cancer cells with a combination of laser light and drugs that makes cancer cells sensitive to light.
Chemotherapy for Skin Cancer
Chemotherapy drugs to kill cancer cells throughout the body and is used if the skin cancer has metastasized and spread to other organs. It is not the standard treatment for this cancer type though unless the cancer has advanced. The treatment is given in cycles of medication and rest to allow the body to recover and reduce the intensity of side effects.
Radiation therapy
Radiation therapy uses high-powered energy beams, such as X-rays, to kill cancer cells. Radiation therapy may be an option when cancer can't be completely removed during surgery.
About bone cancer
Bone cancer occurs when cells in the bone begin to divide uncontrollably and abnormally. Bone cancer can affect any bone in the body, but it most commonly affects the pelvis or the long bones in the arms and legs including thigh bone, knee bone. Bone cancer is a rare type of cancer
Bone cancer is rare-less than 1 percent of all cancers, in addition, bone cancer is not a type of cancer that begins elsewhere in the body and spread to the bone.
There are several treatment options available to cure bone cancer at Oncoplus Hospital, Delhi.
Types of bone cancer
Bone cancer is classified into certain types based on the type of cell where the cancer began. The types of bone cancer include:
- Osteosarcoma: Osteosarcoma is the most common form of bone cancer. In this type, the tumor or cancerous cells form osteoid or bone.
- Primary Osteosarcoma: Tumours that occur between the ages of 15-25 years and affect the sites commonly- the lower-end of the femur; the upper end of the tibia; and the upper end of the humerus.
- Secondary Osteosarcoma: When a premalignant disease affects a bone and develops cancer is termed as secondary osteosarcoma. This type affects people above 45 years.
- Parosteal Osteosarcoma: This type of cancer begins in the region of periosteum.
- Chondrosarcoma: In this type of cancer, the tumor or cancerous cells form cartilage and commonly occurs in the pelvis, legs or arms but is common in flat bones such as ribs, scapula, and ribs.
- Ewing sarcoma: Ewing sarcoma tumors occurs in long bones like tibia and femur and less commonly in flat bones like pelvis. It is more common in teenagers and young adults.
- Fibrosarcoma: Fibrosarcoma is a rare type of cancer that affects cells known as fibroblasts, which are responsible for creating fibrous tissue throughout the body like in tendons(which connect muscle to bone) and other soft tissue like ligaments or muscle.
Signs and Symptoms of Bone Cancer
- Pain in the affected bone
- The affected area may develop swelling and lumps
- Fractures due to weakened bones
- Numbness or a tingling sensation in affected area
- It may cause unintentional weight loss and fatigue
- Difficulty during movement
Book an appointment with the best oncologists for cancer treatment as well as diagnosis at best cancer Hospital in Delhi.
Diagnosis:
Imaging tests can help determine the location and size of bone tumors, and whether the tumors have spread to other parts of the body.
The doctor may advise multiple blood tests to inspect overall general health. Other tissues may include:
- X-ray
- Computed tomography scan
- Magnetic resonance imaging (MRI)
- Positron emission tomography (PET) scan
- Biopsy: A procedure in which tissue samples are removed with a needle or during surgery from the body for examination under a microscope.
WHAT ARE THE CAUSES AND RISK FACTORS OF BONE CANCER?
- Age: Cancers usually appear with age. But in some types of cancers, younger people have a higher risk of developing them.
Osteosarcoma is common in teenagers and young adults and is associated with the growth of bones during puberty. It may also appear in older people.
Spindle cell sarcomas and chondrosarcomas tend to occur in adults between ages 35 and 40 while chondromas occur in adults over 60 years of age. - Radiation therapy or chemotherapy: People who have received radiation or chemotherapy previously run the risk of developing bone cancer, even though it is negligible. If it does occur, it is usually 10-20 years after having radiotherapy. People previously treated with certain chemotherapy drugs might have an increased risk of developing secondary cancer like osteosarcoma.
- Individuals with non-cancerous (benign) bone tumors: Paget’s disease of the bone is a benign condition that causes painful and deformed bones. It mostly occurs in people older than 60 years of age, which results in the formation of abnormal bone tissue. The bones affected are usually dense, thick, brittle and weak. They may be susceptible to a fracture.
- Genetic disorders: People who have inherited a gene that is maladaptive to the bones may run the risk of developing bone cancers. Hereditary retinoblastoma is a rare eye cancer affecting children. They are more susceptible to develop bone cancer (osteosarcoma), soft tissue sarcomas and other cancers.
- Bone Marrow Transplant: Bone marrow transplant is a procedure that replaces bone marrow that is malignant due to infection or chemotherapy. In such cases, there has been an increased risk for developing bone cancers.
WHAT ARE THE STAGES OF BONE CANCER?
Once cancer is diagnosed, tests are recommended to determine the stage of the cancer. Staging is done to find out the severity and extent of cancer spread. Staging helps the specialists to formulate the plan of treatment.
Bone Cancer Treatment Options
The treatment options of bone cancer are based on the type of cancer, the stage of the cancer, patient’s general health. Different bone cancers respond to different treatments, for example, some bone cancers are treated through surgery; some with combination of surgery and chemotherapy; while some with surgery, chemotherapy and radiation therapy.
Chemotherapy in the Treatment of Bone Cancer
Primarily, chemotherapy uses the drugs to destroy the cancerous cells. Chemotherapy drugs are usually delivered through a vein. A few of its primary functions are to starve cancer cells, impede their cell division, and triggering their suicide. While side effects remain, there is an attempt to research drugs that will minimize adverse effects, which are, nausea, weakness, fatigue, bowel-related issues, and blood-related issues, etc.
Radiation Therapy
In Radiation therapy the cancer cells are destroyed using high powered energy radiations. Radiation therapy is often used before an operation because it can shrink the tumour size and make it easier for the surgeon to remove.
Radiation therapy may also be used in patients with bone cancer that cannot be removed through surgery. After surgery, radiation therapy may be used to kill any remaining cancer cells.
Surgery
There are different types of surgery available at Oncoplus Hospital, Delhi for various types and stages of cancer, depending on its size and severity, these are, limb-salvaging surgery, amputation surgery (removal of the limb with affected bone), reconstructive surgery, and surgery for metastasis.
If amputation is needed, you'll likely be fitted with an artificial limb and go through training to learn to do everyday tasks using your new limb.
The goal of surgery is to remove the cancerous tumour completely. In most cases, this involves special techniques to remove the tumor in one single piece, along with a small portion of healthy tissue that surrounds it.
Stem-cell transplants
When Ewing sarcomas are not particularly sensitive to chemotherapy, it may require radiation therapy and perhaps even stem-cell transplants. Stem cell transplants kill bone marrow cells of the affected region, and new cells are induced through the veins to replace destroyed cells through a blood transfusion. Eventually, these new cells adapt to settling down to make healthy bone cells. This process is known as engrafting.
Targeted therapies
Targeted uses drugs to treat cancers but is different from conventional chemotherapy. It works by targeting specific proteins and genes to impede the growth and spread of cancer.
Furthermore, these drugs:
- disable the growth and division of cancer cells
- prevent cells from living longer than usual
- and then, destroy cancer cells
What is Colon cancer
Colon cancer is a type of cancer that begins in the in the rectum or colon present in large intestine. These organs are the final part of the digestive tract. Colon cancer is also called colorectal cancer since it combines colon cancer and rectal cancer that begins in the rectum.
Colon cancer generally affects older adults; however, it can happen at any age. It starts as small and noncancerous polyps that develop inside the colon. Over a period these polyps can develop as colon cancers. That’s why it is suggested to undergo regular screening so as to rule out the disease in early stage, if identified polyps can be removed surgically before these convert into cancer.
Lets check what all are the signs of colon cancer and how it can be managed.
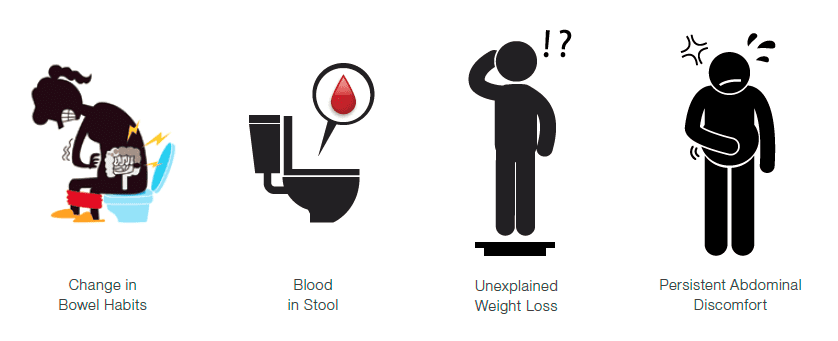
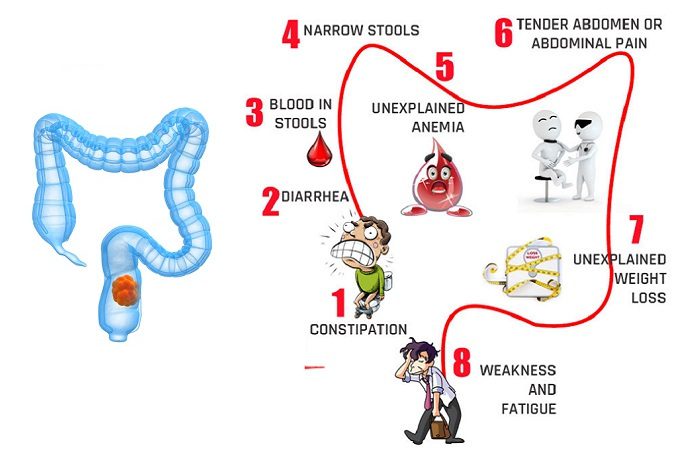
What are the signs and symptoms of colorectal cancer
Generally, patients experience no symptoms in the early stages of the colon cancer. The symptoms appear depending on the cancer's size and location in the large intestine. These symptoms may include:
- A persistent change in bowel habits such as diarrhoea or constipation
- Bleeding per rectum or bloody stool
- Excessive and Persistent discomfort in abdomen such as cramps, gas or pain
- A feeling of incomplete emptying of bowel
- Weight loss without trying
- Weakness
- Excessive bodily fatigue
- Vomiting
Patients may experience the following symptoms in addition in case colon cancer spreads to other parts of the body:
- Jaundice
- Difficulty in breathing
- Swollen Hands or feet
- Long lasting headache
- Blurred vision
- Bone fractures
“We Oncoplus Hospital, Delhi advise patients experiencing early signs to undergo screening before these signs worsen.”
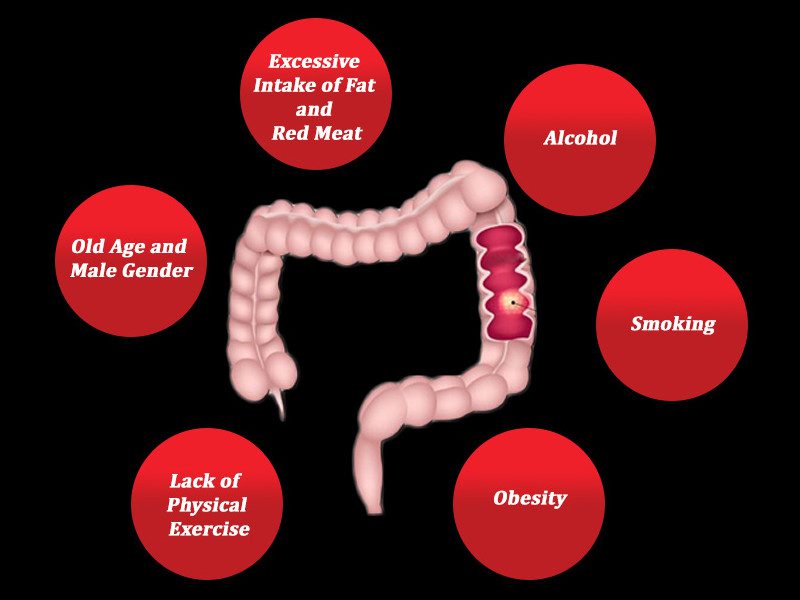
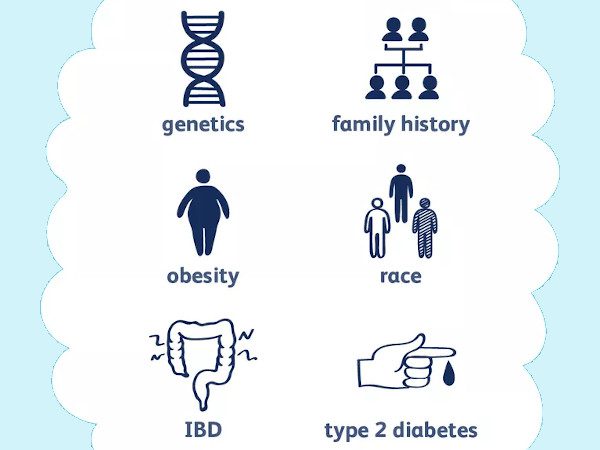
What are the causes of colorectal cancer
Researchers are still working on finding the exact causing factor for colorectal cancer, however there are certain risk factors considered as responsible to contribute I the development of colorectal cancer.
- Gene mutations
Gene mutation is a term used for changes in DNA. When a cell’s DNA is changed or damaged, cells still divide to grow but abnormally developing a tumour. - Precancerous growths
Abnormal cells accumulate in the lining of the colon developing small and non-cancerous polyps. These polyps should be removed surgically to avoid the development of cancerous tumour.
Various risk factors responsible to contribute developing colorectal cancer are as follows:
- Older age: People who are older than 50 are at more risk of developing colorectal cancer.
- Personal history of bowel diseases
- Eating red meats or a diet high in processed foods. Colorectal cancer may be associated with a typical diet, which is low in fiber and high in fat and calories.
- People with a prior history of polyps or colorectal cancer are at a greater risk of colon cancer in the future.
- Inflammatory and chronic conditions of intestine such as ulcerative colitis and Crohn's disease make one at high risk of developing colon cancer.
- Inherited syndromes that are passed through generations can increase colon cancer risk. However, only a small percentage of colon cancers are linked to inherited genes.
- Anyone with a family history of colon cancer is likely to develop colon.
- People with sedentary lifestyle are more likely to develop colon cancer.
- People with diabetes or who are resistant to insulin have an increased risk of colon cancer.
- People who are overweight are at higher risk to develop colon cancer when compared with people considered normal weight.
- Smoking may increase the risk of colon cancer.
- More consumption of alcohol also increases the risk of colon cancer.
Book an appointment with the best oncologists for cancer treatment as well as diagnosis at best cancer Hospital in Delhi.
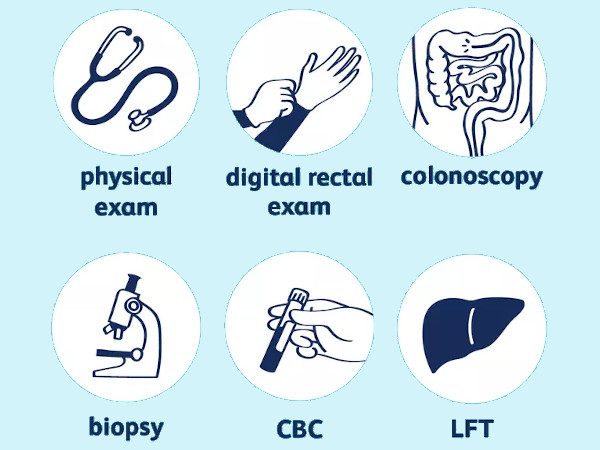
How to diagnose colorectal cancer
There are certain investigations recommended by the experts to screen people with either early signs or no signs in order to look for signs of colon cancer or noncancerous colon polyps. identifying colon cancer at its earliest stage helps the experts to manage the case in real time.
Any screening initiates with a medical and family history of the patient followed by a physical examination. Important tests, which are recommended to rule out the colon cancer are as follows:
- Blood tests: Blood tests do not rule out the have colon cancer, but blood test is required to look for the overall health of the patient such as kidney and liver function tests.
- X-ray
- CT scan: CT scans provides a detailed image of the colon.
- Colonoscopy: It is a procedure that involves the use of a long and flexible tube attached with a small camera. The specialist is able to see inside the colon and rectum to confirm anything unusual. In some cases if doctor finds something unusual, doctor can remove a tissue from abnormal areas which is sent to a laboratory for further analysis.
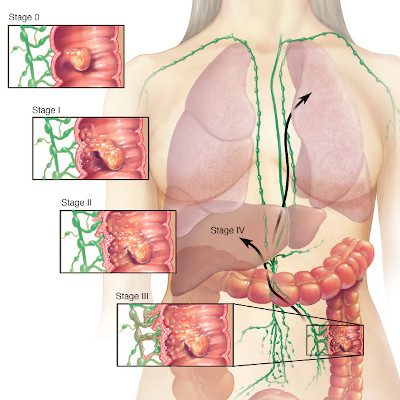
Determining the extent of the cancer
Staging in any cancer helps to determine what treatment options are most suited for a patient. After a thorough evaluation of the patient physically by the expert also through the investigations stages of colorectal cancer can be determined.
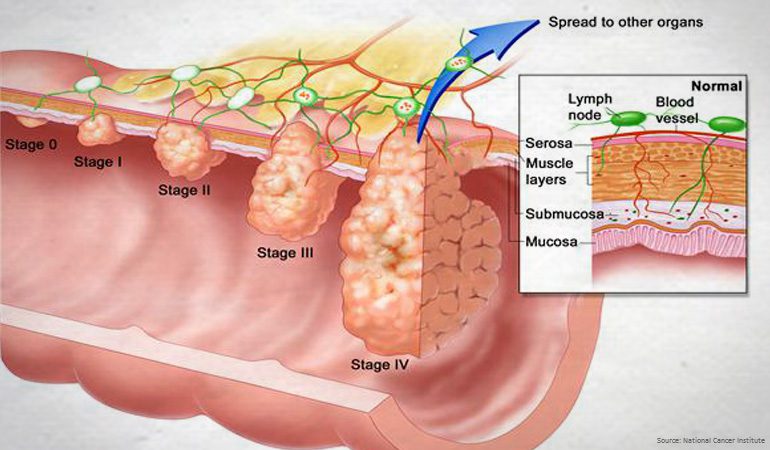
Stages of Colorectal cancer are listed as follows:
Stage 1: This is the early stage where the cancer has penetrated the lining of the colon or rectum but has not spread to the walls of organ.
Stage 2: At this stage, the cancer has spread to the walls of the colon or rectum but has not spread to the lymph nodes or surrounding tissues yet.
Stage 3: At this stage, the cancer has spread to the lymph nodes but not to other parts of the body yet.
Stage 4: This is the most advanced stage also critical one where the cancer has spread to other distant organs, such as the liver or lungs.
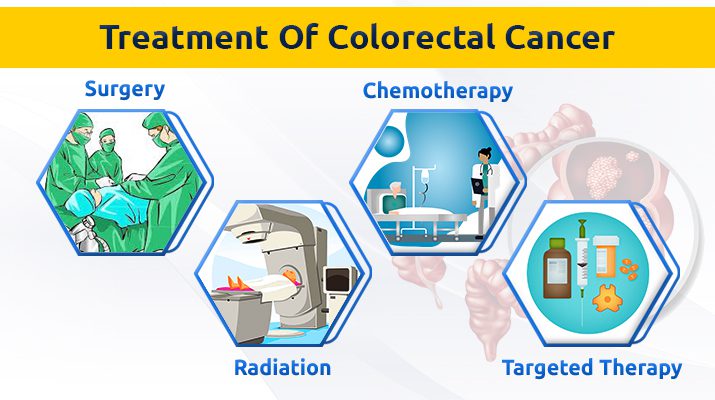
Treatment options for colorectal cancer
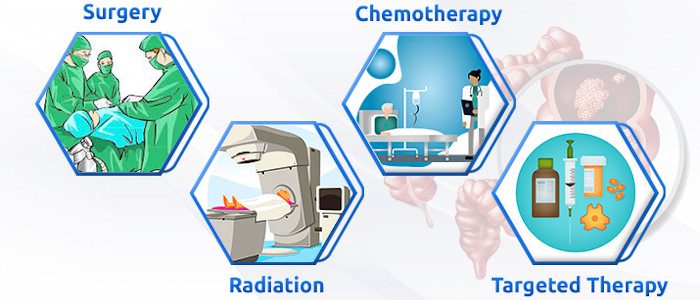
“Various treatment options available at Oncoplus Hospital, Delhi include Surgery, Chemotherapy, Immunotherapy, targeted therapy”. Let us have a detailed look:
Surgery for early-stage colon cancer
- Polypectomy: Surgery done to remove the small and non- cancerous polyp.
- Endoscopic mucosal resection: In this procedure, larger polyps are removed during colonoscopy using special tools.
- Laparoscopic surgery: Those polyps that cannot be removed during a colonoscopy procedure may be removed through laparoscopic surgery.
Surgery for more advanced colon cancer
In case of advanced cancer, surgery is done to relieve a blockage of the colon or other conditions in order to improve the symptoms such as a blockage, bleeding or pain.
In specific cases where the cancer has invaded into the liver or lung but overall health is good, surgery may be recommended to remove the cancer.
But if the cancer has spread to the colon, following surgical procedures are recommended:
- Partial colectomy: This procedure is conducted through laparoscopy. In this procedure, the surgeon removes the part of colon containing the cancer.
- Ostomy: This surgery involves creating a way for waste to excrete through patient’s body. It is carried out by creating an opening in the wall of abdomen from a portion of the remaining bowel for the excretion of stool into a bag that is fitted securely over the opening.
- Colostomy: Is done when patient does not get benefit from Ostomy.
- Lymph node removal: Surrounding lymph nodes are also removed during colon cancer surgery.
Chemotherapy
Chemotherapy uses medicines to kill cancer cells. If the cancer is larger or has spread to the lymph nodes, chemotherapy for colon or rectal cancer is typically given after surgery. After surgery ,chemotherapy may kill any remaining cancer cells in the body and help reduce the risk of cancer recurrence.
In addition, chemotherapy if given before surgery, it might shrink a large cancer so that it is easier to remove with surgery.
Radiation therapy
Radiation therapy uses powerful energy sources to destroy the cancer cells. In some cases, radiation is combined with chemotherapy to enhance the results.
Targeted drug therapy
This type of therapy focus on particular abnormalities present within cancer cells and block these abnormalities eventually killing the cancer cells.
Immunotherapy
Immunotherapy is a type of treatment that uses patient’s immune system to fight cancer. Patients with cancer has weak immune system that may not fight cancer because the cancer cells produce proteins that blind the immune system cells from identifying the cancer cells. Immunotherapy interferes with that process.
Palliative or Supportive care
Palliative care teams aim to improve the quality of life for patients with cancer. This form of care is offered alongside curative or other treatments a patient may be receiving.
Palliative care is specialized medical care that focuses on providing relief from pain and other symptoms of a serious illness. Palliative care is provided by a team of doctors, nurses and other specially trained professionals that work with patient, his/her family and patient’s other doctors to provide an extra layer of support that complements the ongoing care.
Rectal cancer and cancer of colon are often referred to together as "colorectal cancer." But their treatments are quite different because the rectum is situated in a tight space, difficult to separate from other organs and structures in the pelvic cavity.
The rectum is a part of the large intestine that originates at the end of the final segment of the colon and ends when it reaches the short, narrow passage leading to the anus.
Signs and Symptoms of rectal cancer
- Changes in bowel movements like diarrohea or constipation
- Blood and mucus in stool
- Pain in abdomen
- Pain during bowel movements
- Deficiency of iron
- A feeling of incomplete emptying of bowel
- Weight loss for no reason
- Weakness or fatigue
Book an appointment with the best oncologists for cancer treatment as well as diagnosis at best cancer Hospital in Delhi.
Causes and risk factors of rectal cancer
When healthy cells in the rectum make changes in their DNA leading to Rectal cancer. However, in most cases, the cause of such changes in DNA is unknown.
In some cases these changes are inherited that means, these are passed from one generation to another.
One’s lifestyle factors also contribute in development of rectal cancer. These include:
- Old age: People older than 50 years old are at more risk of developing colon and rectal cancer. Colorectal cancer may develop in younger people as well but less frequently.
- Personal history of polyps: Someone who had history of adenomatous polyps, he/she may have a greater risk of colorectal cancer later in life.
- Inflammatory bowel disease: Few chronic inflammatory diseases of the colon and rectum like ulcerative colitis and Crohn's disease, increase the risk of developing the colorectal cancer.
- Family history of colorectal cancer: If someone in family had a history of colorectal cancer, other family members are possibly at risk of developing colorectal Cancer.
- Improper diet: A diet low in vegetables and high in red meat may increase the risk of colorectal cancer.
- A sedentary lifestyle: Anyone with a sedentary lifestyle with no regular physical activity is likely to develop colorectal cancer.
- Diabetes: Diabetes 2 patients may have an increased risk of colorectal cancer.
- Obesity: Obese or overweight people have an increased risk of colorectal cancer associated with risk of dying due to cancer.
- Smoking: Smoking is also considered as one of the risk factors for development of colon cancer.
- Alcohol: Chronic alcohol consumption may increase the risk of colorectal cancer.
- Radiation therapy for previous cancer treatment: Radiation therapy focused at the abdomen for treatment of previous cancers may increase the risk of colorectal cancer.
Diagnosis of rectal cancer
The following blood tests and imaging studies are used as diagnostic tools in rectal cancer:
- CBC-Complete blood count: This test measures the red blood cells count , less number indicates that a tumor is causing blood loss.
- CEA-Carcinoembryonic antigen: In some cases cancers produce substances termed as tumor markers that can be identified in blood. Carcinoembryonic antigen is one such tumour marker, which may be higher in patients with colorectal cancer. Basically CEA test monitors patient’s response to the treatment.
- Chemistry panel: This test checks a number of chemicals in the blood. Abnormal levels of some of these chemicals indicates that cancer has spread to other organs including kidney or liver.
- CT Scan-computed tomography of the chest: This test monitors whether rectal cancer has spread to other organs.
- MRI -magnetic resonance imaging of the pelvis: MRI provides a detailed and clear image of the lymph nodes near the rectum, muscles, organs and other tissues surrounding a tumor in the rectum.
- Colonoscopy: This test is the most precise of all diagnostic investigations. A thin, flexible, lighted tube with a video camera at its tip “known as colonoscope” is used to view the inside of colon and rectum.
Stages of Rectal cancer
Once rectal cancer is diagnosed, the next step is to define the stages of cancer that means to what extent the cancer has spread. Oncologist can decide the appropriate plan of treatment based on the stages. These stages are as follows:
- Stage 0 This is the initial stage of rectum cancer where the cancer cells remain on the surface of the rectal lining(mucosa).
- Stage I At this stage, the cancer extends below the rectal mucosa, penetrating into the rectal wall sometimes.
- Stage II At this stage, cancer extends into or through the rectal wall, grows to the tissues surrounding the rectum.
- Stage III At this stage, cancer cells spread to the lymph nodes near to the rectum, in addition, tumor reach to the structures and tissues outside the rectal wall.
- Stage IV At this stage, cancer has spread to a distant organ or distant lymph nodes.
Treatment options for rectal cancer available at Oncoplus Hospital, Delhi
As other cancers, rectal cancer also require more than one treatment type. Various common treatment options for rectal cancer are:
Surgery is done to remove the tumor, and depends on various factors like:
- Patient’s age
- Patient’s general health
- Patient’s medical history
- The stage of the cancer
- The location of the tumor in the rectum
- The size of the tumor
List of a few surgical procedures commonly used to treat rectal cancer:
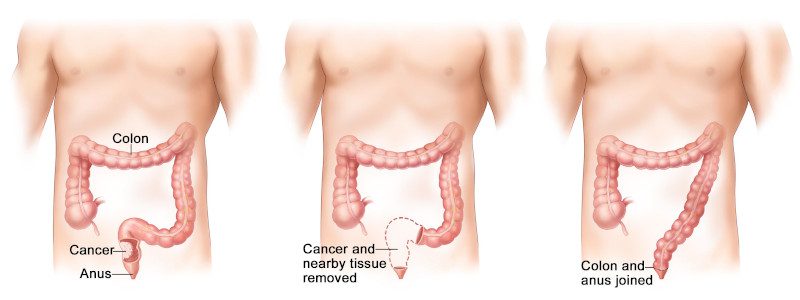
- APR: Abdominoperineal resection with end colostomy. This procedure offers the best treatment for rectal tumors located extremely close to the anal sphincter. With cancer in this location, the surgeon has to remove both the tumor and the sphincter to reduce the risk that the cancer will return.
After APR, it is no longer possible to pass stool through the anus. Stool then passes into a removable pouch placed over the stoma. - Coloanal anastomosis: This procedure may be an option for rectal cancer surgery if the tumor is at least 1 centimeter above the top of the anal sphincter. The surgeon removes the entire rectum and enough of the surrounding tissue to achieve clear margins keeping the anus intact.
- Low anterior resection: Onco-surgeons perform this procedure when the tumor is located in the upper part of the rectum. The surgeon removes the tumor and a margin of healthy tissue around it, leaving the lower part of the rectum in place.
- Local excision: This technique is generally performed for early, small stage 1 rectal cancers, after a biopsy shows that the tumor is unlikely to spread or return. In this procedure, rectal tumor is removed along with a margin of healthy tissue and the section of rectal wall beneath the tumor.
- More-extensive surgery: Patient’s with rectal cancer associated with Crohn's disease, ulcerative colitis or a genetic predisposition to colorectal cancer require surgery that is more extensive than are the procedures explained above.
Chemotherapy
Medicines are given either orally or injected through veins, these medicines kill the cancer cells. Number of sessions given in chemotherapy are decided by the medical Oncologist based on the severity of condition. Chemotherapy is given pre surgery in some cases while in some cases it is given after the surgery.
Target Therapy
Medicines used in this therapy stops the process of changes in DNA.
Combination therapy
Combination of chemotherapy and radiation is a standard treatment for stage II and stage III rectal cancers. This approach is also an option for treating some stage I rectal cancers that have a high risk of recurring.
Palliative care
Palliative care is focused on providing relief from pain and other symptoms of a serious illness. Palliative care specialists work with patient, patient’s family and patient’s other doctors to provide an extra layer of support that complements the ongoing care.
Palliative care is provided by a team of doctors, nurses and other specially trained professionals. Palliative care teams aim to improve the quality of life for patients with cancer and their families.
A mass or growth of abnormal cells in the human brain is called a Brain tumor. There are different types of brain tumors that exist, some are benign i.e, noncancerous while some brain tumors are malignant i.e, cancerous.
Brain tumors can begin in the brain or can begin in other parts of the body and spread to the brain.
Treatment options for brain tumors depend on the type of brain tumor, its size, and location in the body.
Signs and Symptoms OF Brain tumors
The signs and symptoms of a brain tumor depend on the brain tumor’s size, location, and rate of growth. Typical signs and symptoms caused by brain tumors include:
- Headaches that become more frequent and more severe with time
- A change in the pattern of headaches
- Vision problems including blurred vision in some cases or double vision in some cases.
- Loss of movement or sensation in an arm or a leg
- Problems with hearing capacity
- Difficulty with balancing the body
- Difficulties in speech
- Confusion in everyday matters
- Seizures, especially in those who do not have a history of seizures
- Unexplained nausea or vomiting
- Changes in behavior
Book an appointment with the best oncologists for cancer treatment as well as a diagnosis at the best cancer hospital in Delhi.
Causes of Brain tumors
PRIMARY BRAIN tumorS: Brain tumors that originate in the brain are termed primary brain tumors.
There are a few different types of primary brain tumors, each is named after a type of cells involved. Such Primary tumors include:
- Gliomas. These tumors begin in the brain or spinal cord and include astrocytomas, ependymomas, glioblastomas, oligoastrocytomas, and oligodendrogliomas.
- Meningiomas. A meningioma is a tumor that arises from the membranes surrounding our brain and spinal cord (meninges).
- Acoustic neuromas. These are benign tumors that develop on the nerves that control balance and hearing leading from the inner ear to the brain.
- Pituitary adenomas. These are mostly benign tumors that develop in the pituitary gland at the base of the brain.
- Medulloblastomas. These are the most common cancerous brain tumors in children while less common in adults. A medulloblastoma starts in the lower back part of the brain and tends to spread through the spinal fluid.
- Craniopharyngiomas. These type of tumors start near the brain’s pituitary gland that secretes hormones which control many body functions. As the craniopharyngioma grows, it can affect the pituitary gland and other structures near the brain.
SECONDARY BRAIN tumorS: Cancer that begins elsewhere and spreads to the brain are termed as secondary brain tumors. These types of tumors affect people having a history of cancer.
A few cancers that can spread to the brain include:
- Kidney cancer
- Lung cancer
- Breast cancer
- Colon cancer
- Melanoma
Risk Factors of Brain tumors
Some factors are responsible and are identified as risk factors to develop a brain tumor. These include:
- Exposure to radiation. People who are exposed to a type of radiation called ionizing radiation are at more risk of developing brain tumors. Ionizing radiation includes radiation used to treat cancer and radiation released by atomic bombs.
- Family history of brain tumors. People with a family history of brain tumors are at higher risk of brain tumors.
Diagnosis of Brain tumor
- A neurological exam: A neurological exam involves an examination of vision, hearing, balance, coordination, strength, and reflexes. Difficulty or abnormality in one or more areas may indicate which part of the brain could be affected by a brain tumor.
- MRI: Magnetic resonance imaging of the Brain is commonly used as an essential diagnostic tool for brain tumors.
- CT Scans: computerized tomography, Positron emission tomography (PET) may be used for brain imaging.
- BIOPSY: A biopsy can be performed as part of an operation to remove the brain tumor, or a biopsy can be performed using a needle. The biopsy sample is then viewed under a microscope to determine if it is cancerous or benign.
Treatment options available for Brain tumors at Oncoplus Hospital, Delhi
Treatment for a brain tumor is decided on the basis of the type, size, and location of the tumor, as well as the patient’s overall health.
Surgery
If the tumor is located in a place that is accessible for the surgery, Onco-Surgeon removes as much of the brain tumor as possible. As in some cases, tumors are small, in addition, can be separated easily from surrounding brain tissue, such tumors can be removed completely. While in some cases, tumors are located near sensitive areas in the brain or are difficult t separate from surrounding tissue make the surgical intervention risky. In such tumors, Onco-Surgeon removes as much of the tumor as safe. Removal of even a small portion of the tumor may help lessen the signs and symptoms.
Minimally Invasive Scarless Brain Surgery
At Oncoplus Hospital, Delhi, Neurosurgeons are experts in minimally invasive techniques. Our surgical team is able to successfully and safely remove the tumor. Minimal invasive surgeries for brain tumors reduce hospital stay also the recovery is fast.
Radiation Therapy
Radiation therapy uses high-energy X-rays or protons to destroy the cancerous cells.
External beam radiation focuses on that area of the brain where the tumor is located, or in some cases radiation therapy can be focused on the entire brain.
Stereotactic radiosurgery
Stereotactic radiosurgery is not a form of traditional surgery, radiosurgery uses multiple beams of radiation to give a highly focused form of radiation treatment to kill the tumor cells in a very small area. Each beam of radiation is not powerful particularly, but the point where all the beams meet at the brain tumor receives a very large dose of radiation to kill the tumor cells effectively.
Chemotherapy
Chemotherapy uses medicines to destroy cancerous tumor cells. Chemotherapy medicines can be taken orally as pills or can be injected into a vein. Many other chemotherapy medicines are available and may be used depending on the type of cancer.
Targeted Drug Therapy
Targeted drug treatments focus on specific abnormalities present within cancer cells. By blocking these abnormalities, targeted drug treatments can cause cancer cells to die.
Rehabilitation after Brain tumor Treatment
Since brain tumors can affect those parts of the brain that control motor skills, speech, vision, and thinking, hence rehabilitation is a necessary part of the recovery. A few essential therapies are required after brain tumor treatment:
- Physiotherapy to help regain lost motor skills including muscle strength and pain while joints movement.
- Occupational therapy helps the patient get back to his/her normal daily activities including work, after a brain tumor or other related ailment.
- Speech therapy by professional therapists to overcome the difficulty in speaking because of brain tumor.
- Tutoring for school-going children to help children copes with changes in their memory and concentration after a brain tumor.