Rectal cancer and cancer of colon are often referred to together as "colorectal cancer." But their treatments are quite different because the rectum is situated in a tight space, difficult to separate from other organs and structures in the pelvic cavity.
The rectum is a part of the large intestine that originates at the end of the final segment of the colon and ends when it reaches the short, narrow passage leading to the anus.
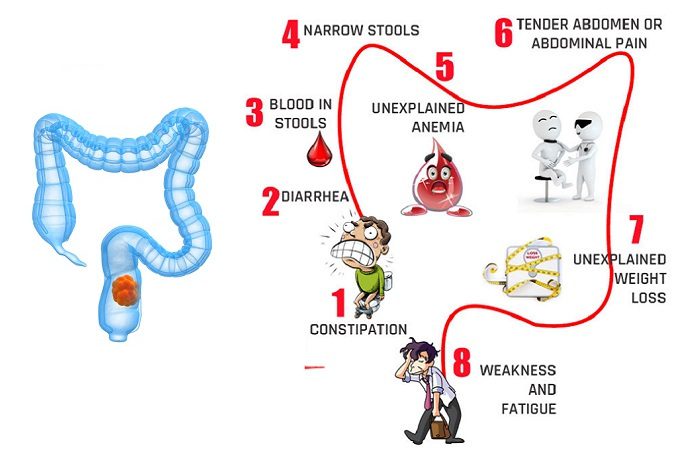
Signs and Symptoms of rectal cancer
- Changes in bowel movements like diarrohea or constipation
- Blood and mucus in stool
- Pain in abdomen
- Pain during bowel movements
- Deficiency of iron
- A feeling of incomplete emptying of bowel
- Weight loss for no reason
- Weakness or fatigue
Book an appointment with the best oncologists for cancer treatment as well as diagnosis at best cancer Hospital in Delhi.
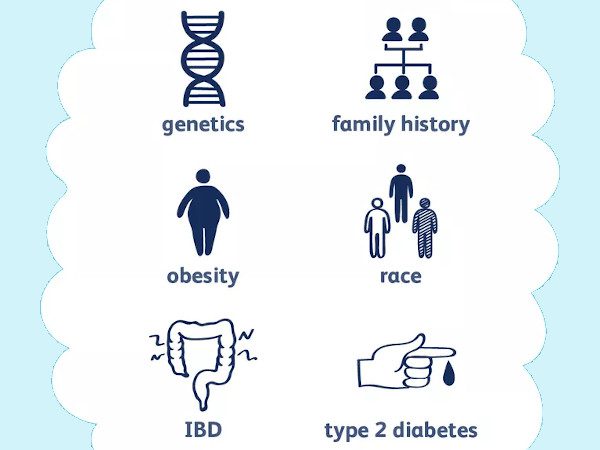
Causes and risk factors of rectal cancer
When healthy cells in the rectum make changes in their DNA leading to Rectal cancer. However, in most cases, the cause of such changes in DNA is unknown.
In some cases these changes are inherited that means, these are passed from one generation to another.
One’s lifestyle factors also contribute in development of rectal cancer. These include:
- Old age: People older than 50 years old are at more risk of developing colon and rectal cancer. Colorectal cancer may develop in younger people as well but less frequently.
- Personal history of polyps: Someone who had history of adenomatous polyps, he/she may have a greater risk of colorectal cancer later in life.
- Inflammatory bowel disease: Few chronic inflammatory diseases of the colon and rectum like ulcerative colitis and Crohn's disease, increase the risk of developing the colorectal cancer.
- Family history of colorectal cancer: If someone in family had a history of colorectal cancer, other family members are possibly at risk of developing colorectal Cancer.
- Improper diet: A diet low in vegetables and high in red meat may increase the risk of colorectal cancer.
- A sedentary lifestyle: Anyone with a sedentary lifestyle with no regular physical activity is likely to develop colorectal cancer.
- Diabetes: Diabetes 2 patients may have an increased risk of colorectal cancer.
- Obesity: Obese or overweight people have an increased risk of colorectal cancer associated with risk of dying due to cancer.
- Smoking: Smoking is also considered as one of the risk factors for development of colon cancer.
- Alcohol: Chronic alcohol consumption may increase the risk of colorectal cancer.
- Radiation therapy for previous cancer treatment: Radiation therapy focused at the abdomen for treatment of previous cancers may increase the risk of colorectal cancer.
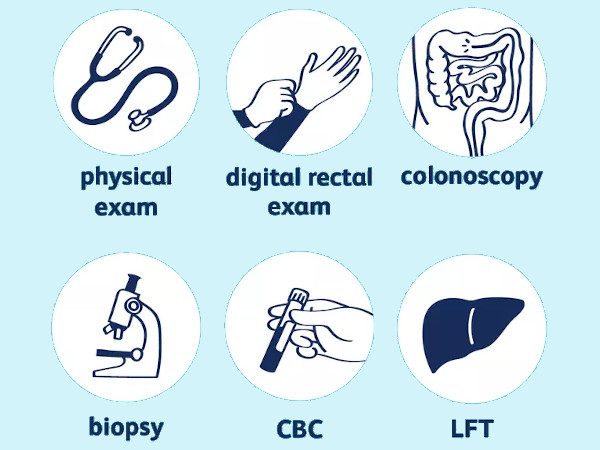
Diagnosis of rectal cancer
The following blood tests and imaging studies are used as diagnostic tools in rectal cancer:
- CBC-Complete blood count: This test measures the red blood cells count , less number indicates that a tumor is causing blood loss.
- CEA-Carcinoembryonic antigen: In some cases cancers produce substances termed as tumor markers that can be identified in blood. Carcinoembryonic antigen is one such tumour marker, which may be higher in patients with colorectal cancer. Basically CEA test monitors patient’s response to the treatment.
- Chemistry panel: This test checks a number of chemicals in the blood. Abnormal levels of some of these chemicals indicates that cancer has spread to other organs including kidney or liver.
- CT Scan-computed tomography of the chest: This test monitors whether rectal cancer has spread to other organs.
- MRI -magnetic resonance imaging of the pelvis: MRI provides a detailed and clear image of the lymph nodes near the rectum, muscles, organs and other tissues surrounding a tumor in the rectum.
- Colonoscopy: This test is the most precise of all diagnostic investigations. A thin, flexible, lighted tube with a video camera at its tip “known as colonoscope” is used to view the inside of colon and rectum.
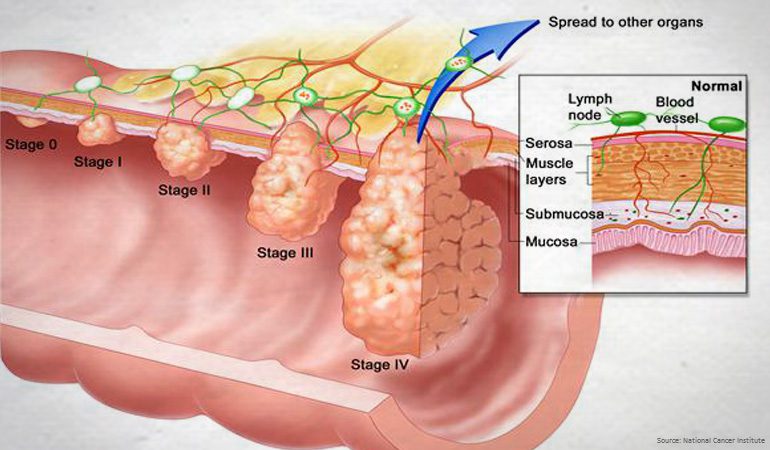
Stages of Rectal cancer
Once rectal cancer is diagnosed, the next step is to define the stages of cancer that means to what extent the cancer has spread. Oncologist can decide the appropriate plan of treatment based on the stages. These stages are as follows:
- Stage 0 This is the initial stage of rectum cancer where the cancer cells remain on the surface of the rectal lining(mucosa).
- Stage I At this stage, the cancer extends below the rectal mucosa, penetrating into the rectal wall sometimes.
- Stage II At this stage, cancer extends into or through the rectal wall, grows to the tissues surrounding the rectum.
- Stage III At this stage, cancer cells spread to the lymph nodes near to the rectum, in addition, tumor reach to the structures and tissues outside the rectal wall.
- Stage IV At this stage, cancer has spread to a distant organ or distant lymph nodes.
Treatment options for rectal cancer available at Oncoplus Hospital, Delhi
As other cancers, rectal cancer also require more than one treatment type. Various common treatment options for rectal cancer are:
Surgery is done to remove the tumor, and depends on various factors like:
- Patient’s age
- Patient’s general health
- Patient’s medical history
- The stage of the cancer
- The location of the tumor in the rectum
- The size of the tumor
List of a few surgical procedures commonly used to treat rectal cancer:
- APR: Abdominoperineal resection with end colostomy. This procedure offers the best treatment for rectal tumors located extremely close to the anal sphincter. With cancer in this location, the surgeon has to remove both the tumor and the sphincter to reduce the risk that the cancer will return.
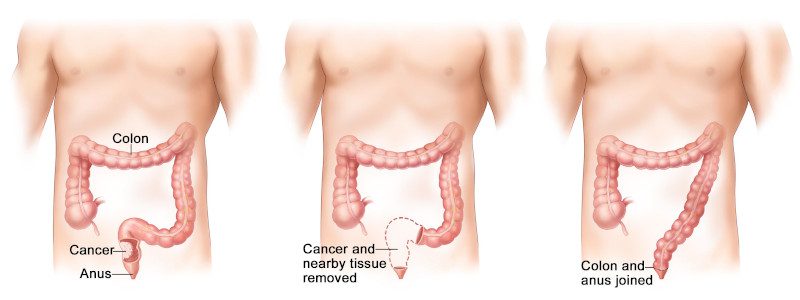
After APR, it is no longer possible to pass stool through the anus. Stool then passes into a removable pouch placed over the stoma. - Coloanal anastomosis: This procedure may be an option for rectal cancer surgery if the tumor is at least 1 centimeter above the top of the anal sphincter. The surgeon removes the entire rectum and enough of the surrounding tissue to achieve clear margins keeping the anus intact.
- Low anterior resection: Onco-surgeons perform this procedure when the tumor is located in the upper part of the rectum. The surgeon removes the tumor and a margin of healthy tissue around it, leaving the lower part of the rectum in place.
- Local excision: This technique is generally performed for early, small stage 1 rectal cancers, after a biopsy shows that the tumor is unlikely to spread or return. In this procedure, rectal tumor is removed along with a margin of healthy tissue and the section of rectal wall beneath the tumor.
- More-extensive surgery: Patient’s with rectal cancer associated with Crohn's disease, ulcerative colitis or a genetic predisposition to colorectal cancer require surgery that is more extensive than are the procedures explained above.
Chemotherapy
Medicines are given either orally or injected through veins, these medicines kill the cancer cells. Number of sessions given in chemotherapy are decided by the medical Oncologist based on the severity of condition. Chemotherapy is given pre surgery in some cases while in some cases it is given after the surgery.
Target Therapy
Medicines used in this therapy stops the process of changes in DNA.
Combination therapy
Combination of chemotherapy and radiation is a standard treatment for stage II and stage III rectal cancers. This approach is also an option for treating some stage I rectal cancers that have a high risk of recurring.
Palliative care
Palliative care is focused on providing relief from pain and other symptoms of a serious illness. Palliative care specialists work with patient, patient’s family and patient’s other doctors to provide an extra layer of support that complements the ongoing care.
Palliative care is provided by a team of doctors, nurses and other specially trained professionals. Palliative care teams aim to improve the quality of life for patients with cancer and their families.