Understanding the pancreas and its disease acute pancreatitis
Understanding the pancreas and its disease acute pancreatitis
- onco
- November 26, 2024
The pancreas, a small yet crucial organ, plays an essential role in both digestion and regulation of blood sugar levels. It may be small in size, but its functions have a profound impact on our overall health. When the pancreas becomes inflamed, it can lead to a severe condition known as acute pancreatitis, a condition that can range from mild discomfort to life-threatening complications. In this blog post, we will explore the structure and function of the pancreas, the causes and symptoms of acute pancreatitis, how the condition is diagnosed, and the pancreatic cancer treatment options available for those who are affected.
The Role of the Pancreas
The pancreas is a gland that sits behind the stomach, between the spleen and the duodenum, which is the first segment of the small intestine. It resembles a tapering leaf or fish and is roughly six inches long. Despite its relatively small size, the pancreas performs critical functions in two major areas: digestion and hormone regulation.
What is Acute Pancreatitis?
Acute pancreatitis is an inflammation of the pancreas that occurs suddenly and typically causes severe abdominal pain. Unlike chronic pancreatitis, which develops over time and can cause long-term damage to the pancreas, acute pancreatitis is a short-term condition ranging from mild to severe, with symptoms often appearing suddenly and without warning.
In acute pancreatitis, the digestive enzymes that the pancreas produces typically to break down food become prematurely activated while still inside the pancreas. This can lead to the pancreas beginning to “digest” itself, causing tissue damage, inflammation, and swelling. The inflammation can spread to other organs in severe cases, leading to widespread complications.
Read More Blog: Living With Pancreatic Cancer.. Terminal Illness As A Turning Point!
Causes of Acute Pancreatitis
Acute pancreatitis can occur for a variety of reasons. Here are some of the most typical explanations given below:
Gallstones – Gallstones are a common cause of acute pancreatitis that can block the bile duct, which connects the gallbladder to the pancreas, leading to a backup of digestive fluids. This can cause the enzymes to activate prematurely and begin digesting the pancreas.
Chronic and Heavy Alcohol Use – Excessive alcohol consumption is another significant risk factor for acute pancreatitis. Alcohol can irritate the pancreas and lead to inflammation, especially if consumed in large quantities over time. This is particularly dangerous because it can increase the likelihood of developing both acute and chronic pancreatitis.
High Blood Triglycerides – Elevated levels of triglycerides (a type of fat found in the blood) can lead to the development of acute pancreatitis. This condition is often associated with metabolic syndrome or uncontrolled diabetes.
Medications – Certain medications can cause an allergic or toxic reaction that leads to pancreatitis. Some chemotherapy drugs, corticosteroids, and medications used to treat high blood pressure and diabetes are among those that have been linked to pancreatitis.
Abdominal Trauma – Physical injury or surgery to the abdomen can sometimes lead to acute pancreatitis. This can occur if the pancreas is damaged directly or if there is an issue with bile or pancreatic ducts being obstructed.
Infections – Certain viral infections, such as mumps or hepatitis, can lead to pancreas inflammation. In rare cases, bacterial infections can also trigger acute pancreatitis.
Genetic Factors – Some people have genetic mutations that predispose them to acute pancreatitis, even without other risk factors like alcohol use or gallstones.
Symptoms of Acute Pancreatitis
The symptoms of acute pancreatitis can range from mild to severe and typically appear suddenly. Common symptoms include:
Severe Abdominal Pain – The most common and prominent symptom is a sharp, intense pain in the upper abdomen that often radiates to the back. The pain may worsen while lying down or after having a meal.
Nausea and Vomiting – Many people with acute pancreatitis experience nausea and vomiting, which can exacerbate dehydration.
Fever – A mild to moderate fever may develop as a response to inflammation in the body.
Increased Heart Rate – Tachycardia, or a fast heart rate, can occur due to pain or dehydration.
Abdominal Tenderness and Bloating – The abdomen may become swollen or tender to the touch due to inflammation and the buildup of fluid in the abdominal cavity.
In more severe cases, complications such as shock, organ failure, or infected pancreatic tissue can arise, leading to more severe symptoms such as confusion, low blood pressure, and respiratory distress.
Read More Blog: Dealing With Pancreatic Cancer, Expert Opinion
Diagnosis of Acute Pancreatitis
If a person exhibits symptoms of acute pancreatitis, prompt diagnosis and treatment are crucial. To confirm the diagnosis, healthcare providers may perform the following:
Blood Tests – Blood tests are the most common diagnostic tool for acute pancreatitis. Elevated levels of pancreatic enzymes such as lipase and amylase may be a sign of pancreatic inflammation.
Imaging – An abdominal ultrasound, CT scan, or MRI may be used to examine the pancreas and look for signs of inflammation, gallstones, or other complications.
Endoscopic Ultrasound (EUS) – In some cases, a doctor may use an endoscope to view the pancreas more closely and check for issues such as blocked bile ducts or gallstones.
Treatment of Acute Pancreatitis
The severity of acute pancreatitis typically determines the course of treatment. Most cases of mild acute pancreatitis resolve with supportive care, while severe cases may require more intensive medical intervention.
Hospitalization – In most cases, individuals with acute pancreatitis need to be hospitalized, often for several days, to monitor their condition and manage complications.
Fasting – The patient may be asked to refrain from eating or drinking to allow the pancreas time to rest and heal. In some cases, intravenous fluids and nutrients may be provided to prevent dehydration and malnutrition.
Pain Management – Relieving pain is a crucial component of therapy. Pain can be managed with medications, including nonsteroidal anti-inflammatory drugs (NSAIDs) or opioids for severe pain.
IV Fluids – Dehydration is a common complication of acute pancreatitis, and intravenous fluids are essential to keep the body hydrated and maintain blood pressure.
Treating the Underlying Cause – If the pancreatitis is caused by gallstones, medications or surgery may be needed to remove the stones or clear the bile ducts. If alcohol is the cause, the patient will need to stop drinking alcohol completely, and additional support may be required to address alcohol dependence.
Surgery or Endoscopic Procedures – In rare cases, surgery or endoscopic procedures may be required to remove damaged tissue, drain fluid collections, or address blocked ducts.
The pancreas plays a crucial role in digestion and the regulation of blood sugar, and its inflammation, as seen in acute pancreatitis, can have serious consequences. While acute pancreatitis can often be managed with timely intervention and supportive care, its severity can range from mild to life-threatening. Understanding the pancreas and the factors that contribute to acute pancreatitis is essential for prevention, early detection, and effective treatment. If you experience acute pancreatitis symptoms, seeking immediate medical attention is vital to avoid complications and improve outcomes. Immune system recovery after chemo is a critical part of the healing process, as chemotherapy can weaken the body’s natural defence mechanisms. Oncoplus offers advanced support to help restore immune function, promoting faster recovery and enhancing overall well-being during post-treatment recovery.
Recent Posts
-
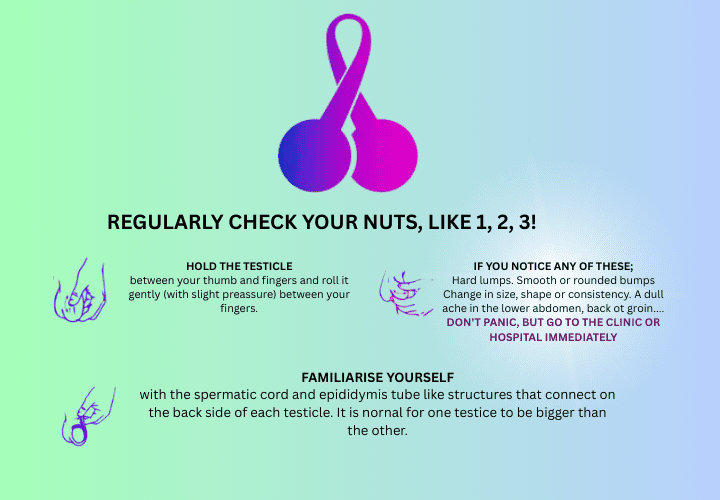
Can Testicular Cancer affect fertility?
April 23, 2025
-
Why are Breast Cancer Cases Increasing Around the World?
April 17, 2025

Leave a Reply